Fetal ductal arteriosus (DA) restriction is an important but often misunderstood fetal cardiovascular condition. This article outlines an objective, physiology‑based approach to screening, diagnosis, severity assessment, and management, integrating Doppler findings with right ventricular (RV) response.
1. What is Fetal Ductal Arteriosus Restriction?
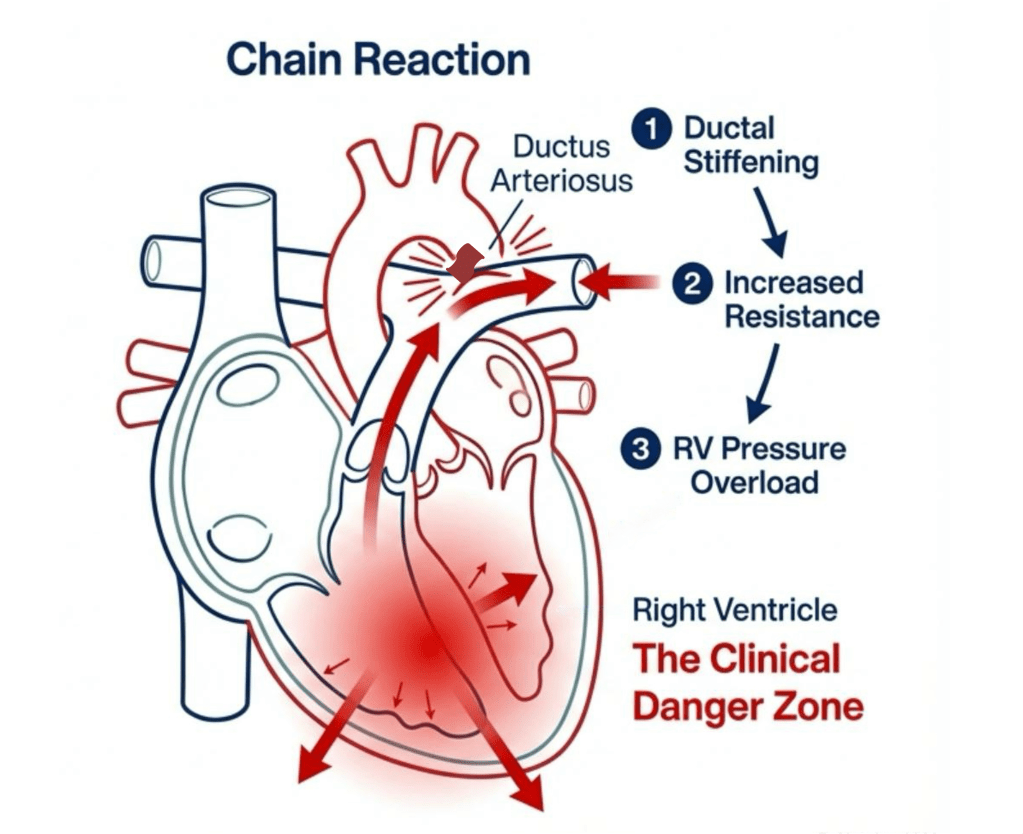
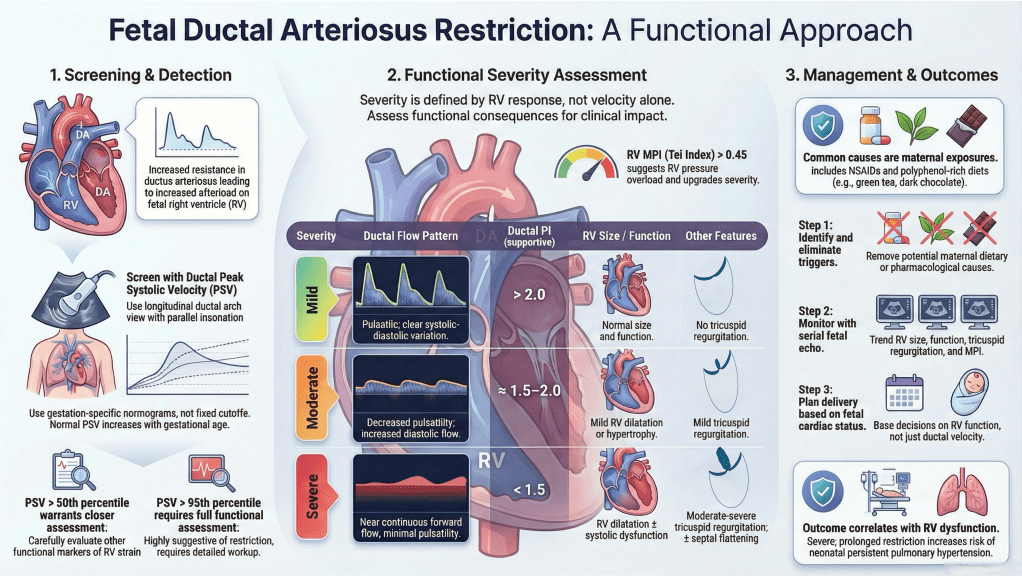
Fetal ductal arteriosus restriction refers to increased resistance to flow through the ductus arteriosus before birth. It is primarily a functional abnormality caused by ductal stiffening or constriction, leading to increased RV afterload. Anatomical narrowing usually appears later in the disease process.

2. How is it Detected?
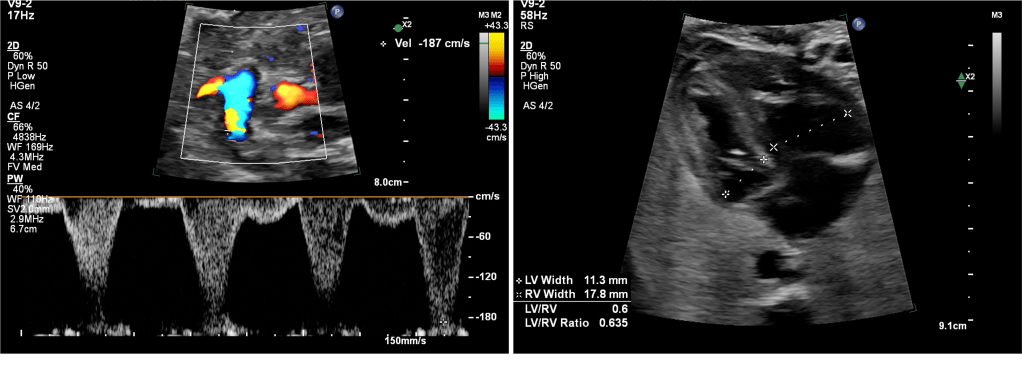
Detection relies on Doppler assessment of ductal flow and evaluation of the fetal right heart. Key elements include ductal peak systolic velocity (PSV), pulsatility, diastolic flow, and secondary RV changes.
3. Velocity-Based Screening Using a Normogram
Ductal PSV increases physiologically with gestational age. Therefore, screening should be based on gestation‑specific percentile curves rather than fixed velocity cutoffs. Values up to the 95th percentile may be physiologic in the absence of functional abnormalities. Once velocities exceed the 50th percentile, careful assessment of other markers is recommended.
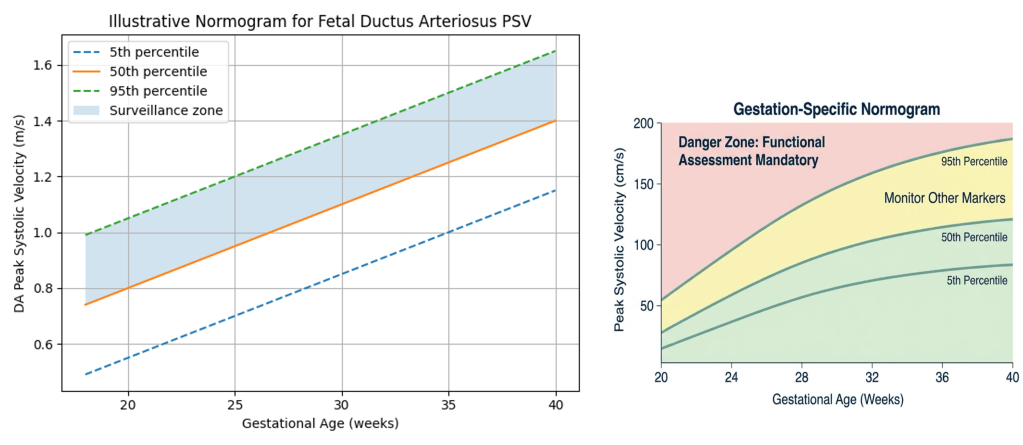
Illustrative gestation‑specific normogram for DA PSV. Velocities above the 95th percentile should prompt functional assessment.
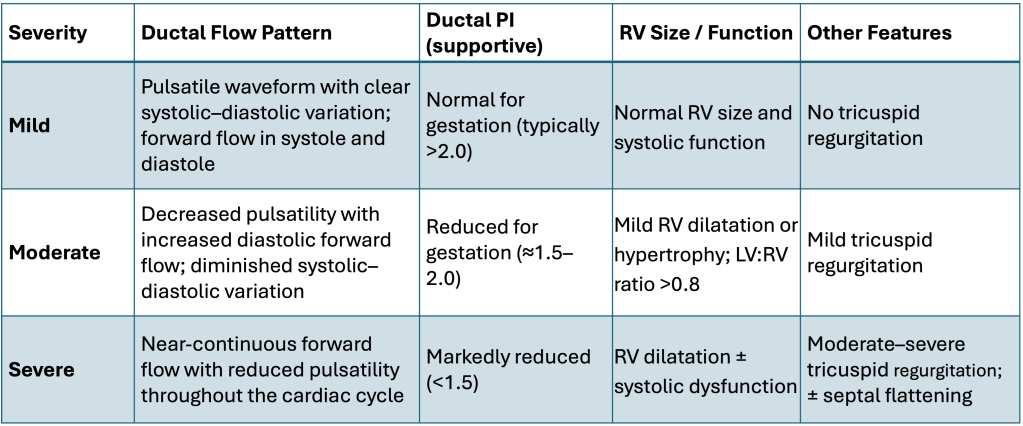
4. Functional Severity Assessment
Severity is defined by functional consequences rather than velocity alone.
• Mild: Preserved pulsatility, forward systolic and diastolic flow, normal RV size and function.
• Moderate: Reduced pulsatility, shortened diastolic flow, mild RV hypertrophy or tricuspid regurgitation (TR).
• Severe: Minimal or absent diastolic flow, non‑pulsatile waveform, RV dilatation or dysfunction, moderate–severe TR.
Role of Myocardial Performance Index (MPI)
Right ventricular MPI (Tei index) provides an objective measure of global RV function. In the absence of robust gestation‑specific cutoffs, an MPI value above approximately 0.45 is considered suggestive of RV pressure overload and should upgrade severity classification.
Role of Pulmonary Vein Doppler
Pulmonary vein Doppler may provide indirect information on left atrial filling and pulmonary venous congestion. However, there is insufficient validated data to recommend its routine use in diagnosing or grading fetal ductal arteriosus restriction. Its role remains adjunctive and primarily research‑oriented.
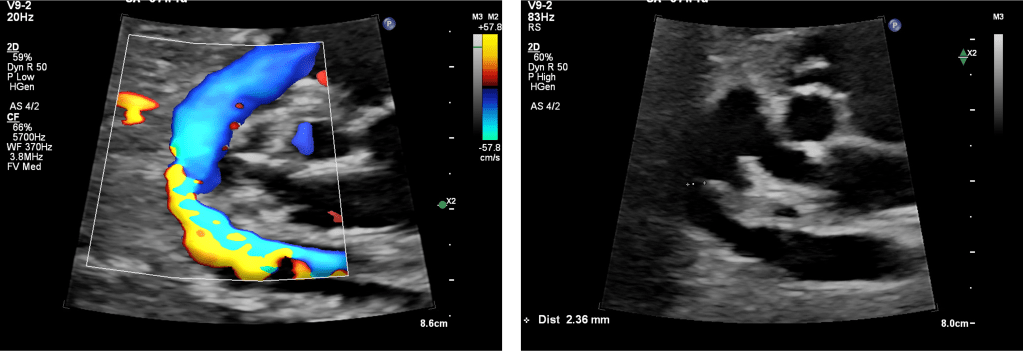
5. Ductal Arch View: Practical Imaging Recommendations
• Use a longitudinal ductal arch view of the fetus.
• Ensure near‑parallel insonation.
• Avoid oblique sampling from the three‑vessel trachea view alone.
• Assess flow pattern, not velocity alone.
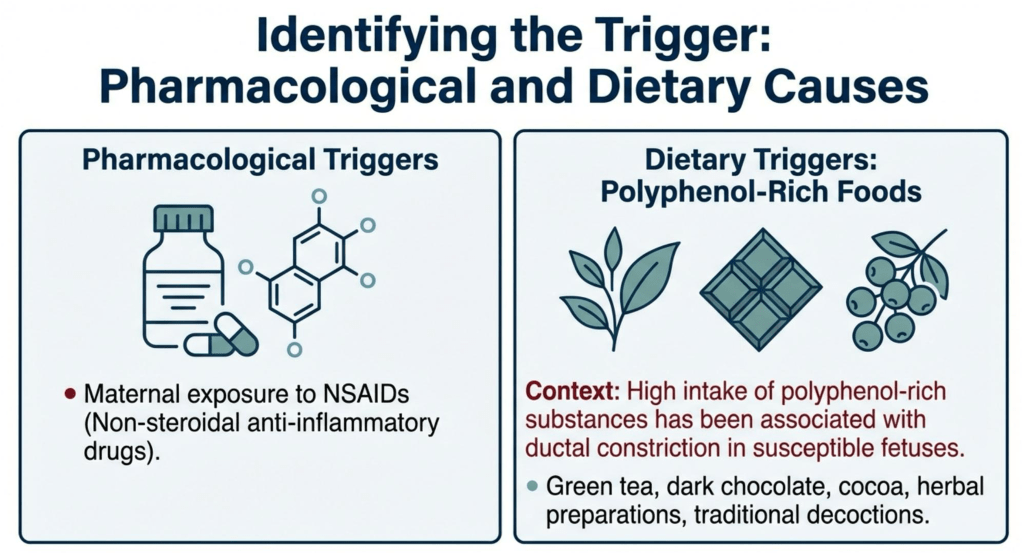
6. Causes and Risk Factors
Common causes include maternal exposure to NSAIDs and polyphenol‑rich diets. In the Indian context, high intake of green tea, dark chocolate, cocoa, certain herbal preparations, and traditional decoctions has been associated with ductal constriction in susceptible fetuses.
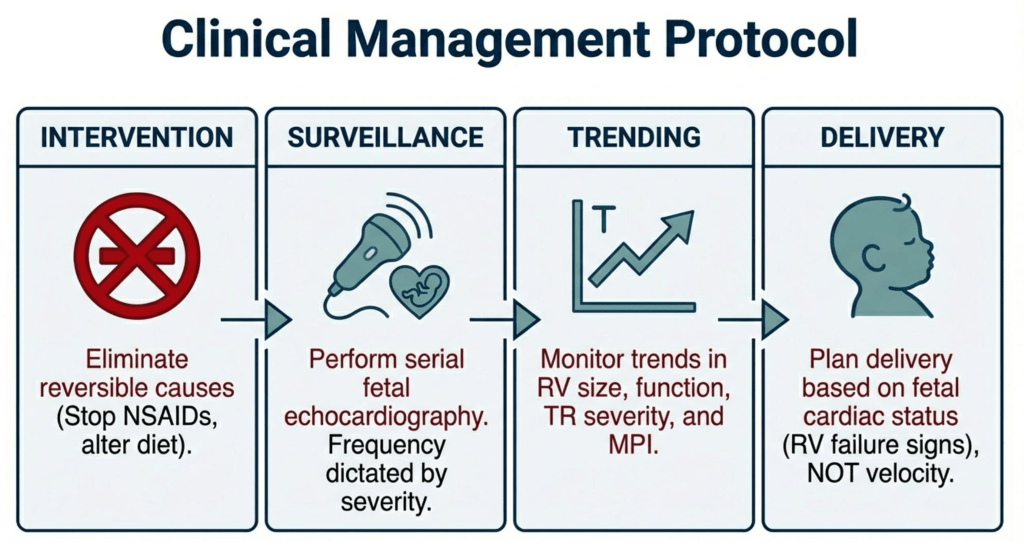
7. Management Protocol
1. Identify and eliminate reversible causes.
2. Perform serial fetal echocardiography based on severity.
3. Follow RV size, function, TR, and MPI trends.
4. Plan delivery based on fetal cardiac status rather than velocity alone.
8. Outcomes
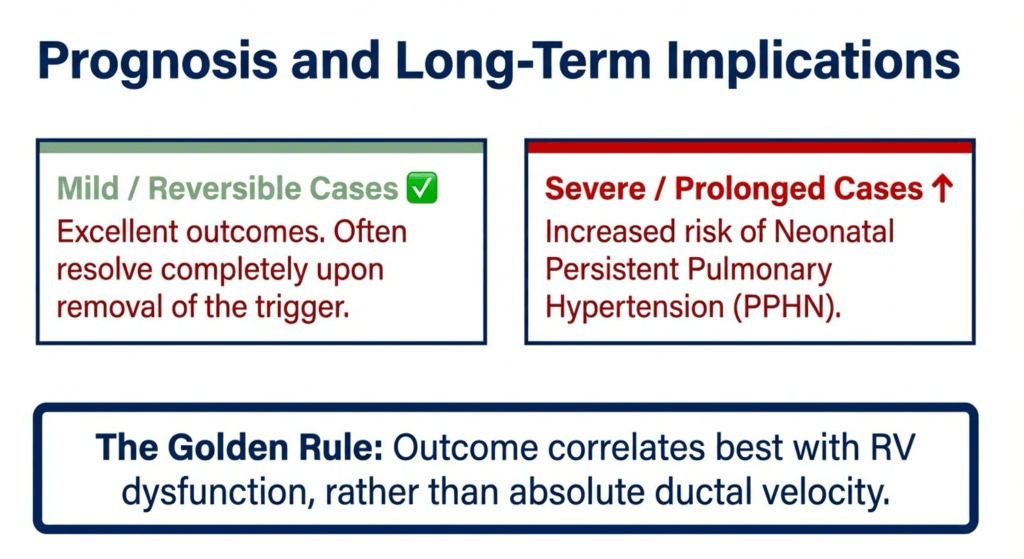
Mild cases often resolve with the removal of the trigger and have excellent outcomes. Severe or prolonged restriction increases the risk of neonatal persistent pulmonary hypertension. Outcome correlates best with RV dysfunction rather than absolute ductal velocity.
Summary
Audio Summary
Suggested reading
1. Mielke G, Benda N. Reference ranges for ductus arteriosus Doppler flow velocities. Ultrasound Obstet Gynecol.
2. Mori Y et al. Fetal ductal constriction and right ventricular Tei index. Am J Cardiol.
3. Zielinsky P et al. Fetal ductal constriction: diagnosis and management. J Am Soc Echocardiogr.
4. ISUOG Practice Guidelines: Fetal Cardiac Examination.
