The timing of fetal echocardiography is central to accurate diagnosis, meaningful counselling, and planning pregnancy management. Although early cardiac assessment is possible, the most reliable and comprehensive evaluation is achieved between 18–22 weeks, when cardiac size, acoustic windows, and anatomical development are optimally aligned.
One of the immediate considerations after diagnosing a significant congenital heart defect is whether the family wishes to continue the pregnancy. This is where the local legal framework for medical termination of pregnancy becomes relevant. Each region has its own limits and procedural requirements, which directly influence the amount of time parents have to understand the condition, complete genetic evaluation, and make an informed decision. The aim, therefore, is to reach a clear and decisive diagnosis well within the legal window, ensuring families have access to the full range of options available to them.
The Ideal Window: Comprehensive Transabdominal Fetal Echocardiography
The recommended timing for a full fetal echocardiographic anatomic survey is 18–22 weeks.

So during this window:
- The fetal heart reaches an ideal size for detailed assessment, with excellent resolution for both chambers and outflow tracts.
- Rib and spinal ossification is still incomplete, resulting in minimal acoustic shadowing and clearer thoracic windows.
- Amniotic fluid volume and a thin fetal chest wall provide favourable ultrasound penetration.
- Cardiac orientation is stable enough to obtain all standard views consistently.
- Doppler signals are reliable due to more mature and steadier fetal hemodynamics.
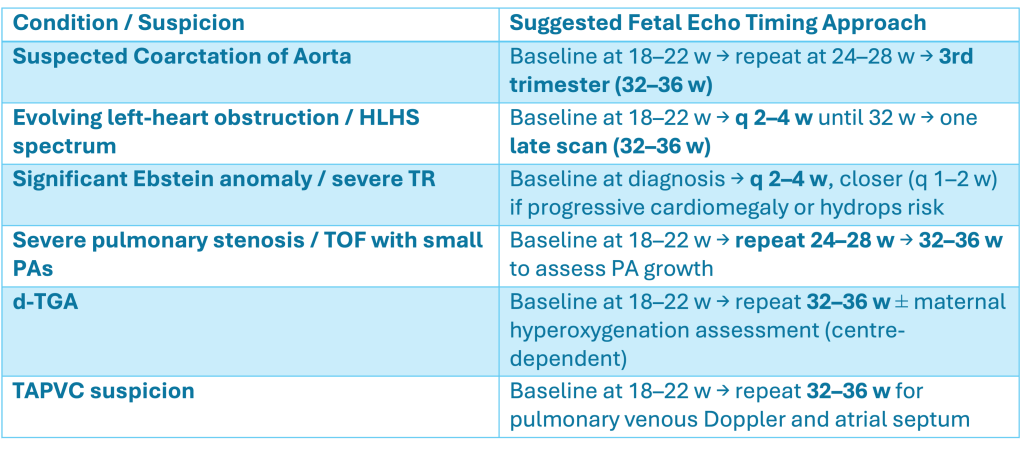
Even with optimal timing, a few lesions (e.g., coarctation, evolving outflow obstruction, small VSDs) may present later. This is why strategic follow-up scans remain important in selected pregnancies.
Early Fetal Echocardiography (11–16 Weeks)
Early targeted fetal echocardiography—performed in the late first trimester (11–13+6 weeks) or early second trimester (14–16 weeks)—has become increasingly feasible with high-resolution equipment.
When to offer an early scan
- Increased nuchal translucency
- Abnormal first-trimester screening
- Positive family history of CHD
- Suspected cardiac abnormality on early obstetric scan
- Known high-risk genetic background
What early scans can and cannot do
- They can detect many severe lesions early, especially outflow tract abnormalities and AV septal defects.
- They cannot replace the 18–22-week comprehensive study.
- Sensitivity depends on equipment, operator experience, and fetal position.
- The smaller heart limits full anatomical detail.
Need for repeat scan
Every early fetal echo, normal or abnormal, requires confirmation at 18–22 weeks.
If there is residual suspicion, a 24–28-week follow-up helps assess evolving lesions such as coarctation or valve obstruction.
Transvaginal Fetal Echocardiography
Transvaginal imaging is an excellent adjunct, especially in the first trimester.
Indications
- Suboptimal transabdominal views in early gestation
- Very early targeted evaluation at 11–13+6 weeks
- Suspicion of major CHD where higher resolution is needed
Advantages
- Superior image quality at small gestations
- Better Doppler and structural detail early in pregnancy
Limitations
- Requires specific expertise
- More invasive than transabdominal scanning
- Findings still need confirmation by the 18–22-week comprehensive scan
The MTP Act in India: Why Timing Matters
Once a significant congenital heart defect is diagnosed, a key consideration is whether the family wishes to continue the pregnancy.This decision is shaped by the legal framework of the region, and in India, the MTP Act is particularly relevant, as outlined below.
The MTP (Amendment) Act 2021 expanded access and added pathways for termination in the context of fetal abnormalities.
Current MTP Act 2021 – Major Provisions
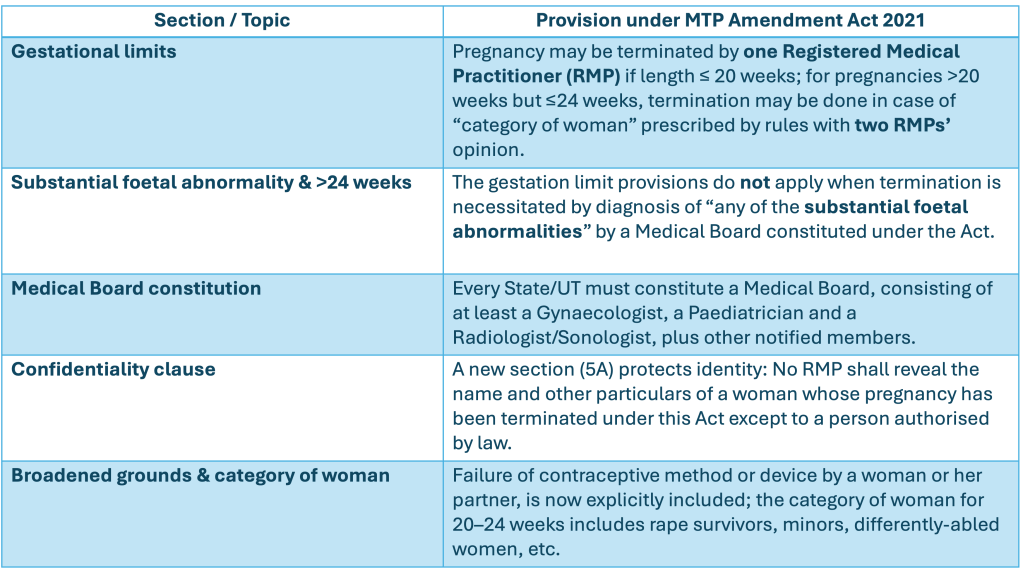
Key Changes from the Previous Act (MTP Act 1971)
- Upper gestation limit extension: The previous Act allowed termination up to 20 weeks; the Amendment raised it to 24 weeks for defined categories of women.
- Medical Board for >24 weeks & foetal anomaly: Earlier, there was essentially no provision for termination beyond 20 weeks except in extreme life-threatening cases; now termination beyond 24 weeks is legally available if a Medical Board certifies substantial fetal abnormality.
- Confidentiality and broader grounds: The Amendment introduced explicit confidentiality protections and expanded the grounds, compared with the 1971 Act.
For cardiac anomalies, this means:
- Detecting major CHD before 20–24 weeks is crucial to allow families the full range of options.
- Clear documentation, timely referral, and coordinated counselling are essential.
- When significant abnormalities are detected late, Medical Board approval may be required.
Genetic Testing: Practical Timing in the Real World
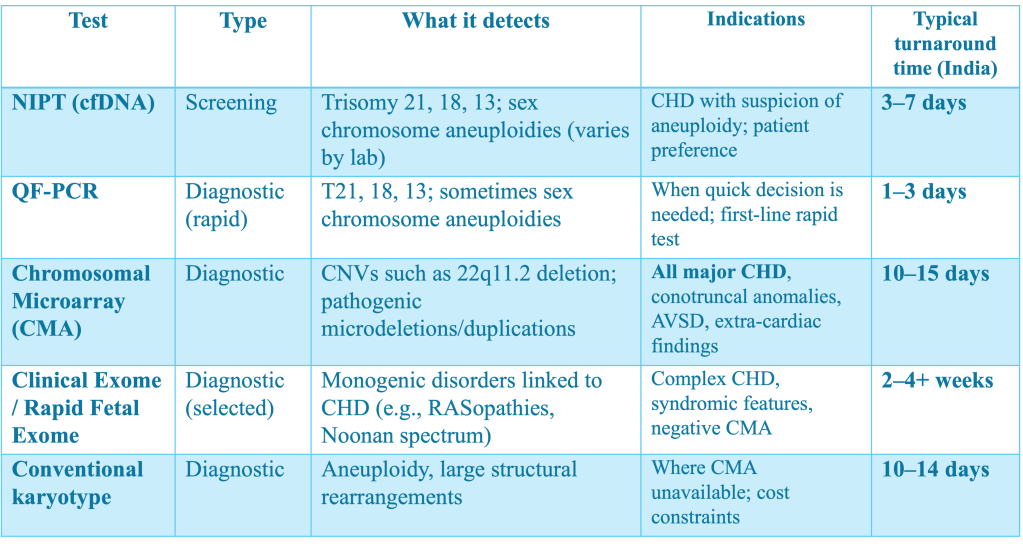
Genetic evaluation plays a major role in the work-up of fetal heart disease. Decision-making is often time-sensitive, so understanding test types and turnaround times helps in planning.
Commonly used prenatal genetic tests
- Rapid aneuploidy tests (QF-PCR) – Fastest diagnostic option
- NIPT (cfDNA) – A screening tool, not diagnostic
- Chromosomal microarray (CMA) – Best first-line diagnostic test for structural anomalies
- Exome sequencing – Useful in selected cases but time-consuming
Prenatal Genetic Testing in Fetal Cardiac Disease
When to Repeat or Review a Fetal Echocardiogram
A review scan is recommended when:
- Early fetal echo was done → repeat at 18–22 weeks.
- Suspicious or borderline findings → reassess at 24–28 weeks.
- Lesions affecting perinatal management are present
- Urgent findings on routine obstetric ultrasound → review within 48–72 hours.
- Genetic results alter risk assessment → repeat as appropriate.
Maternal Anti-Ro/La or Previous CHB

CHD-Related Serial Monitoring Needs
Take-home message
A well-timed fetal echocardiography pathway, anchored on the 18–22-week comprehensive scan, supported by early targeted and transvaginal imaging, and integrated with genetic testing and MTP timelines, ensures that families receive timely, accurate and compassionate care.

