Fetal echocardiography allows detailed assessment of fetal cardiac structure, rhythm, and function. Early diagnosis of congenital heart disease (CHD) improves perinatal planning, counseling, and timely intervention — particularly for duct-dependent or complex lesions.
Because universal fetal echocardiography is not yet practical in most settings, referral is guided by specific maternal, fetal, and genetic indications. These recommendations reflect current evidence and major guidelines (ASE 2023, ISUOG 2023, AIUM/ACOG).
This document presents a concise, evidence-based framework for when to perform fetal echocardiography, along with risk-stratified guidance for clinical practice.
Principles of Indication Classification
The likelihood of fetal CHD depends on a combination of maternal, fetal, and familial risk factors.
- Maternal factors: medical conditions, autoimmune antibodies, teratogens
- Fetal findings: ultrasound abnormalities, increased NT, arrhythmias
- Familial/genetic factors: previous child with CHD, parental CHD, chromosomal abnormalities
- Functional assessment — cardiac output, ventricular function, MPI, venous/arterial Dopplers, and surveillance for evolving hydrops
- Parental request for reassurance: based on parental anxiety or preference after appropriate counselling
- Extended care / clinical vigilance: may be considered even without classical risk factors, as CHD can occur in otherwise low-risk pregnancies, also when imaging views are suboptimal or when there is heightened clinical suspicion,
The goal is simple: identify pregnancies where the likelihood of CHD is several times higher than baseline, without overloading the system with unnecessary referrals.
A. Maternal Indications

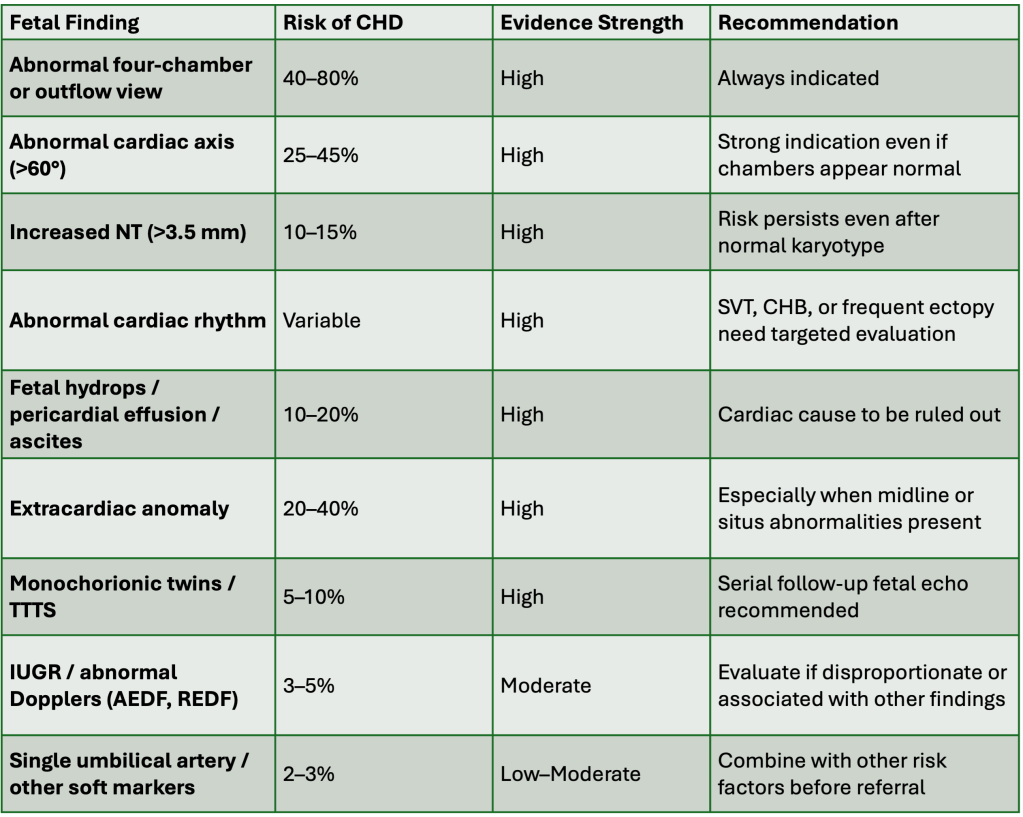
B. Fetal Ultrasound Findings
C. Familial / Genetic Indications

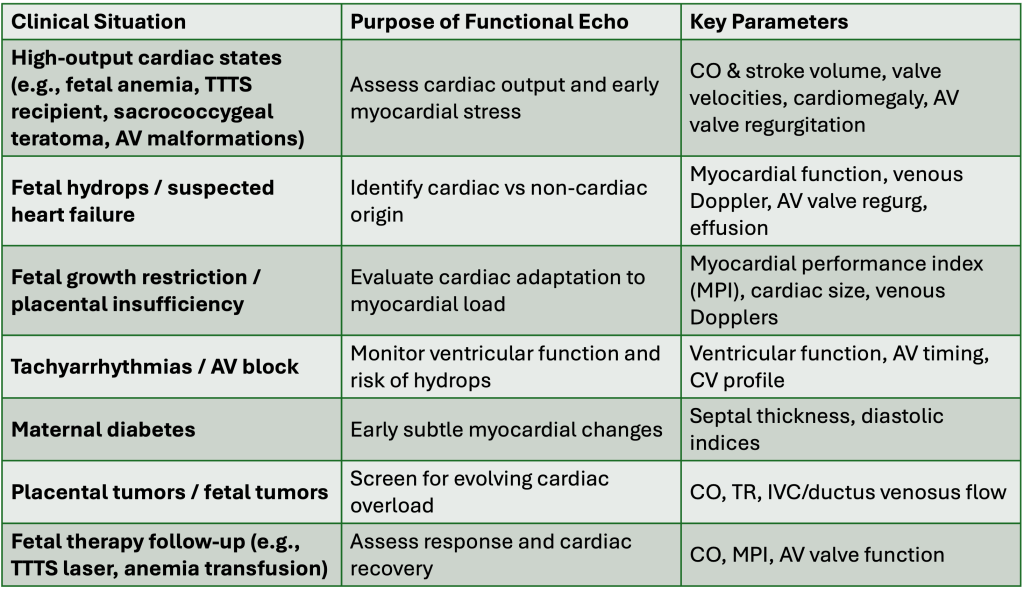
D. Functional Assessment Indications (Hemodynamic Evaluation)
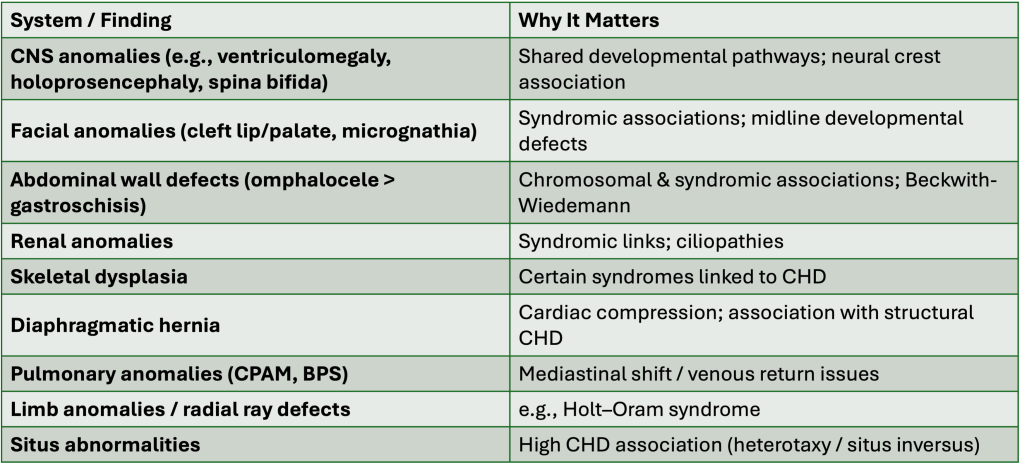
E. Extracardiac Anomalies Associated with CHD (an extension Fetal Ultrasound Findings)
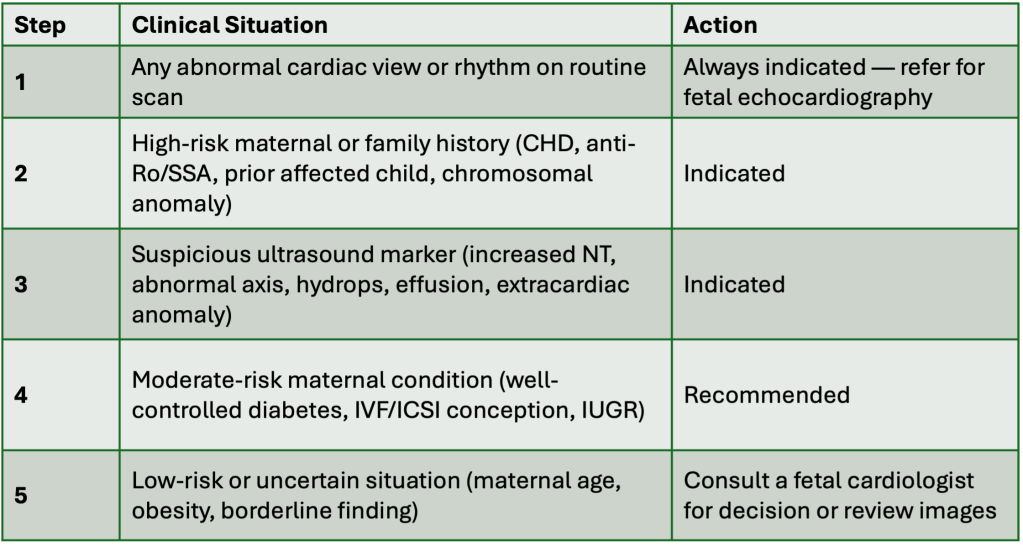
Suggested Risk Stratification
Risk is not uniform. Some conditions carry high (≥5x baseline) risk, while others have modest (≈2x) or uncertain risk.

A Note About “No Risk Factors”
Interestingly, more than half of all fetuses with CHD have no known risk factor.
A normal maternal history does not ensure a normal heart.
That’s why high-quality routine obstetric cardiac screening — proper four-chamber and outflow views — remains essential.
When imaging is technically limited or the fetal position is unfavorable, a targeted fetal echocardiogram can still be valuable even in an apparently low-risk pregnancy.
Parent-Driven Request
While indication-based referral remains standard, it is important to acknowledge that a significant number of parents may choose fetal echocardiography electively, even without major risk factors.
Common reasons include:
- Desire for reassurance
- Previous adverse pregnancy anxiety
- Limited clarity on routine ultrasound views
- Higher awareness and access to care
In such situations, fetal echocardiography may be offered after appropriate counselling, provided there is no medical contraindication and expectations are clear.
“Sometimes, reassurance itself is a valid clinical need.”
A normal fetal echo in a worried family can reduce anxiety and support pregnancy bonding and preparedness.
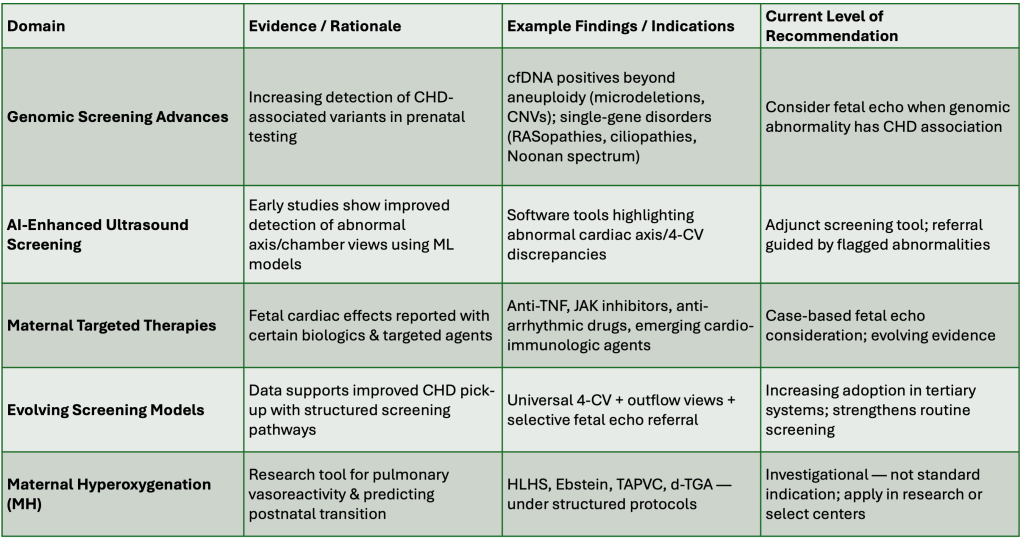
G. Emerging and Expanding Indications
Timing and Follow-Up
- Routine fetal echo: 18–22 weeks gestation
- Early scan (12–16 weeks): for high-risk cases such as maternal CHD, raised NT, or anti-Ro antibodies
- Serial follow-up: when progressive or dynamic lesions are suspected (e.g., AV block, TTTS)
- Repeat study: if early imaging was suboptimal or new findings appear
Summary: “Who Should Get a Fetal Echocardiography?”
Conclusion
As fetal cardiac care evolves with better imaging, genetics, and screening tools, our approach must stay structured yet flexible. Indications define who must be scanned, but real-world practice also values clinical intuition, image quality, and parent engagement.
A thoughtful referral pathway, supported by fetal cardiology expertise, ensures babies with heart disease are recognised early and cared for with attention, planning, and compassion.
We screen to find, but we prepare to protect — and that is where fetal echocardiography makes its greatest impact.

