1. Introduction
The fetal Myocardial Performance Index MPI) is a valuable tool in the range of functional fetal echocardiography. It goes beyond standard anatomical assessment by offering a dynamic, quantitative measure of both systolic and diastolic ventricular function. MPI acts as a key marker for identifying subclinical myocardial dysfunction well before overt cardiac failure or hydrops develop.
2. What is MPI & Why Both Systolic/Diastolic Assessment
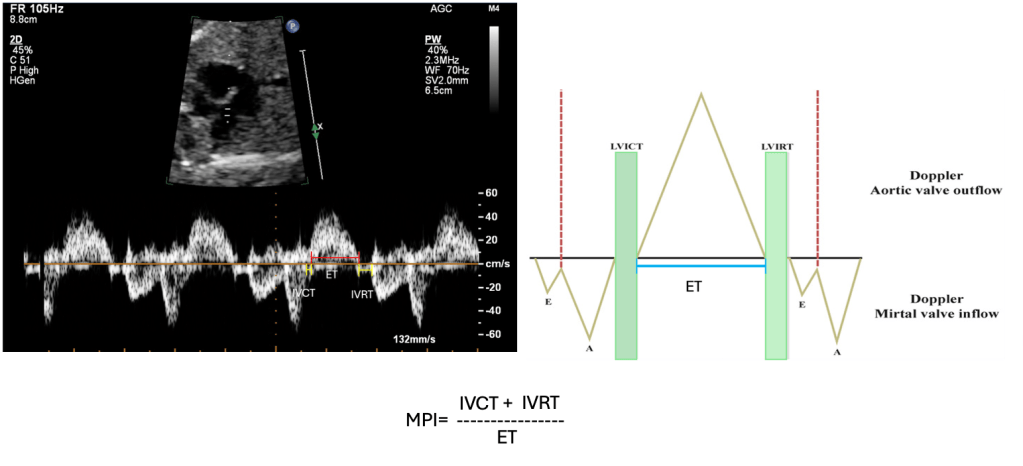
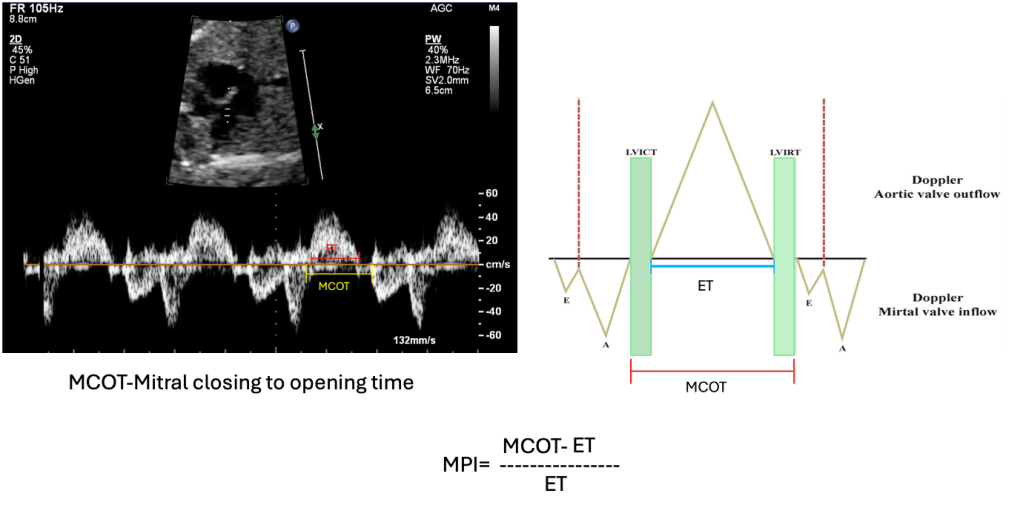
The Modified Myocardial Performance Index is a load-independent Doppler-derived metric that reflects combined systolic and diastolic myocardial performance by analysing key parts of the cardiac cycle:
- Isovolumetric Contraction Time (ICT): The interval after atrioventricular valve closure and before semilunar valve opening, representing ventricular contraction buildup
- Isovolumetric Relaxation Time (IRT): The period after semilunar valve closure and before atrioventricular valve opening, reflecting ventricular relaxation
- Ejection Time (ET): The duration of active ventricular blood ejection
The formula is: (IVCT+IVRT)/ET
This captures both ventricular contraction (systolic) and filling (diastolic) phases in a single index.
The Modified Myocardial Performance Index is a term used when valve clicks are used as landmarks for measuring time intervals (Hernandez-Andrade et al.).
Extensive adult studies demonstrate that MPI’s relative independence from heart rate and loading makes it particularly suited for high fetal heart rates and variable circulatory conditions.
3. Pathophysiology: Dual Mechanisms
Functional impairment detected by MPI arises from two main mechanistic pathways:
- Acute Mechanism: Reversible Ca²⁺ handling dysfunction involving impaired SERCA2a activity and disrupted sarcoplasmic reticulum calcium reuptake. This delays ventricular relaxation and the onset of contraction, prolonging ICT and IRT.
- Chronic Mechanism: Persistent fibrotic remodelling mediated by TGF-β1, endothelin-1, and reactive oxygen species. Results in collagen deposition, myocardial stiffening, and contractile protein loss, causing sustained systolic and diastolic dysfunction.
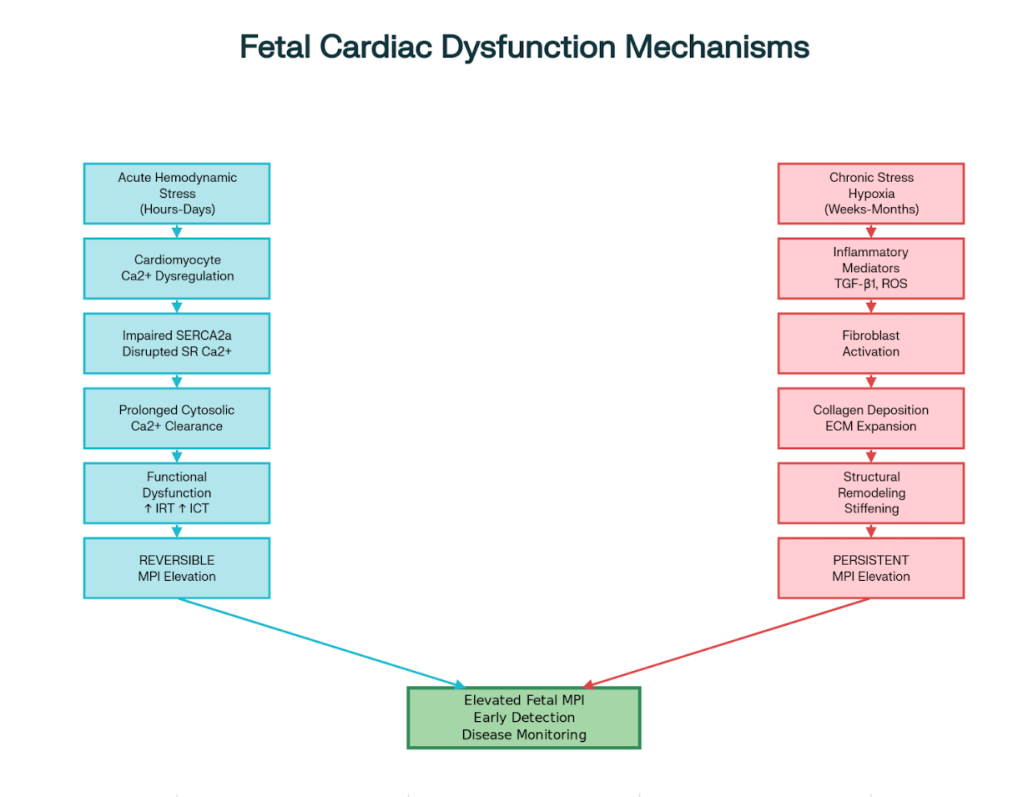
Understanding these mechanisms informs the clinical interpretation of MPI changes, distinguishing early functional disturbances from advanced structural damage.
4. Technical Methodology
Accurate MPI measurement requires:
- Imaging a four-chamber Aortic view (5-C view), with the Doppler sample volume positioned on the aortic wall near the mitral valve
- Sample volume size of 2–3 mm and insonation angle under 15° for optimal signal fidelity
- Doppler settings: sweep speed 15 cm/s, wall motion filter between 120–300 Hz, and gain minimised to reduce noise
- Identification of valve clicks as landmarks for measuring ICT, IRT, and ET ensures reproducibility
- Analysis of at least three consecutive cardiac cycles for better results.
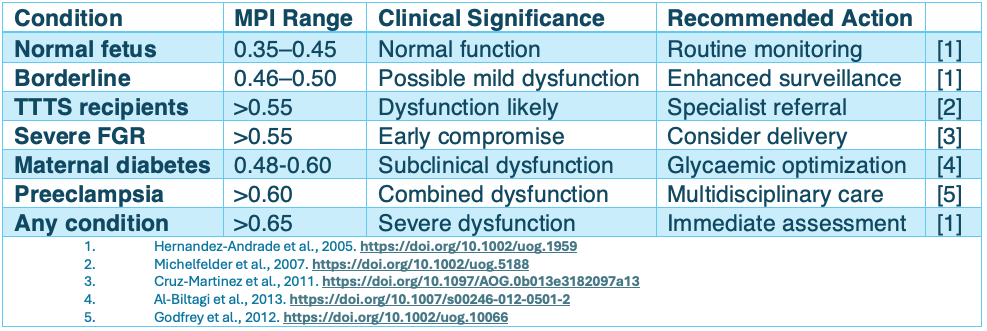
5. Normal Reference Values
MPI values vary by population and gestational age, but typically range:
- Approximately 0.35–0.45 in normal fetuses from mid to late gestation
- Slightly higher ranges reported in certain ethnic groups (e.g., 0.42–0.45 in Asian cohorts)
Interpretation thresholds:
- 0.46–0.55: Mild dysfunction, warrants enhanced monitoring
- 0.56–0.65: Moderate dysfunction, potential indication for intervention
- 0.65: Severe dysfunction, urgent clinical assessment required
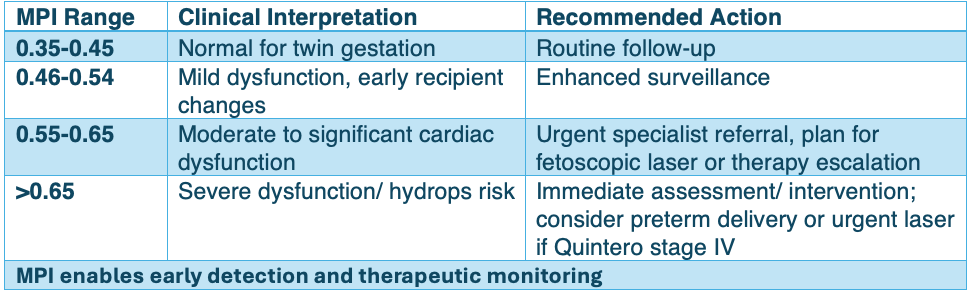
6. Practical Clinical Reference
7. Clinical Applications: MPI Values in Disease States
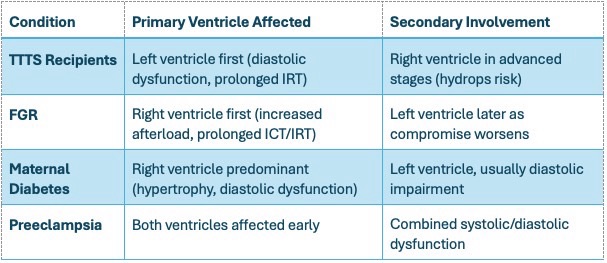
Twin-to-Twin Transfusion Syndrome (TTTS)
TTTS represents the most extensively studied application of fetal MPI assessment:
Recipient Twins:
- Baseline MPI: 0.55–0.75 (significantly elevated)
- Primary mechanism: Prolonged IRT reflecting diastolic dysfunction
- Post-laser therapy: Normalisation within 4 weeks in successful cases
Donor Twins:
- Baseline: Often normal (0.32–0.42) or slightly reduced
- Post-therapy: May develop transient elevation due to circulatory readjustment
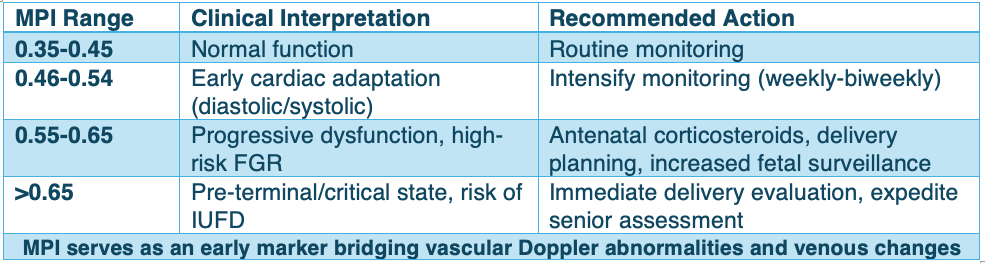
Fetal Growth Restriction (FGR)
FGR demonstrates progressive cardiac dysfunction correlating with severity:
- Early FGR: MPI 0.50–0.62 (predominantly diastolic dysfunction)
- Severe FGR with AEDF: Values >0.65 associated with poor perinatal outcomes
- Mechanism: Prolonged IRT and ICT reflecting both diastolic and systolic impairment
- Clinical utility: Early detection of cardiac compromise before overt heart failure
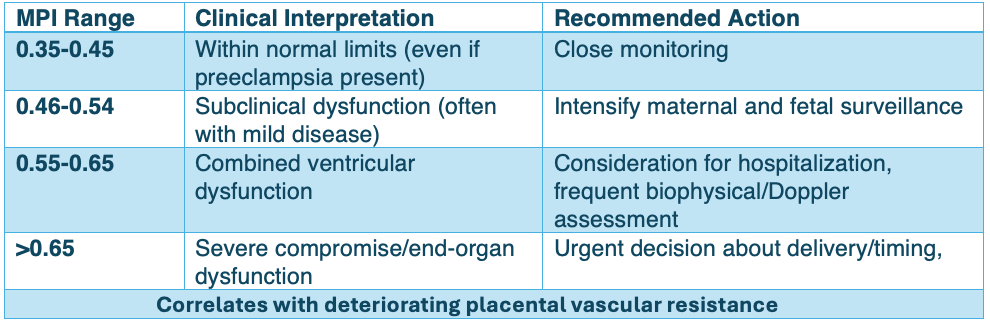
Preeclampsia
Severe preeclampsia demonstrates a significant cardiac impact:
- MPI elevation: 0.55–0.70 (irrespective of growth restriction presence)
- Progressive worsening: Correlates with deteriorating placental vascular resistance
- Both ventricles affected: Combined systolic and diastolic dysfunction
Maternal Diabetes
Diabetic pregnancies show consistent patterns of fetal cardiac dysfunction:
Gestational Diabetes:
- MPI range: 0.45–0.58 (elevated compared to controls)
- Primary change: Diastolic dysfunction with prolonged IRT
- Onset: Detectable as early as the first trimester in poorly controlled cases
Pre-gestational Diabetes:
- More severe elevation: 0.48–0.65, depending on glycemic control
- HbA1c correlation: Higher values are associated with worse MPI
- Mechanism: Hyperinsulinemia-induced myocardial hypertrophy and dysfunction
Integration with other parameters maximises predictive accuracy. Fetal echo, including MPI, is therefore indispensable for comprehensive management.
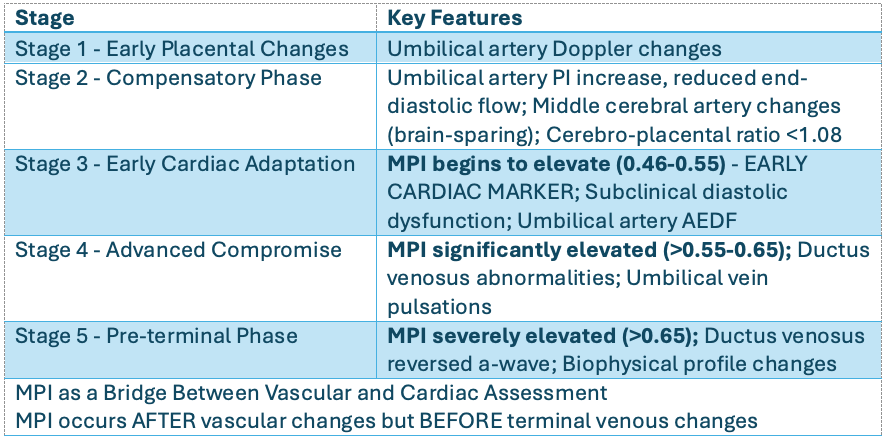
Sequential Changes in Placental Insufficien
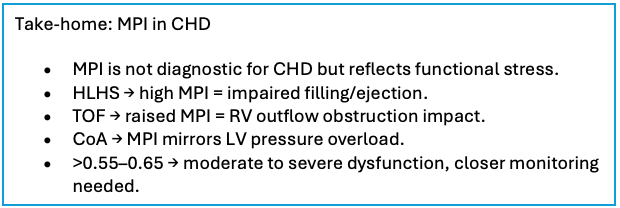
8. MPI in CHD
MPI is not a primary diagnostic tool for congenital heart disease, but its values can vary with different lesions and provide useful functional insights. In HLHS, elevated MPI reflects impaired filling and ejection, helping with risk stratification and delivery planning. In TOF, right ventricular outflow obstruction often raises MPI, supporting decisions on timing of intervention. In Coarctation of the Aorta, MPI changes mirror left ventricular pressure overload and can help in monitoring progression. Although disease-specific cut-offs are not well defined, persistently high MPI values in the moderate-to-severe range (>0.55–0.65) suggest significant dysfunction and warrant closer surveillance. This remains an evolving area, and I will continue to update as further research emerges on the role of MPI in CHD.
Right vs. Left Ventricular MPI
While all the discussion of MPI is about LV MPI by default, it is important to remember that the right ventricle often bears the greater burden in fetal compromise, especially in conditions like fetal growth restriction and maternal diabetes. Assessing RV MPI can therefore add valuable functional insights, and it becomes particularly relevant in lesions such as HLHS or pulmonary stenosis. In routine practice, though, LV MPI is still more widely used because it is easier to measure and has stronger reference data. Encouragingly, a few recent studies using automated techniques for RV MPI show promising results, and in the future, RV MPI may become part of standard assessment; at least in selected indications.
9. Caveats & Limitations
- Operator dependence and technical demands limit widespread use
- Lack of universal reference ranges, influenced by population and methodology
- Limited ability to differentiate systolic vs diastolic dysfunction in isolation
- Extreme loading or heart rates may influence MPI
- Requires incorporation into multimodal fetal cardiac assessment
10. Conclusion
MPI is a crucial, multifaceted tool in fetal cardiac assessment, enabling the early identification of myocardial dysfunction across various pathologies and informing clinical management with actionable data. Its integration into routine fetal echocardiography represents progress toward functional evaluation that complements anatomical diagnosis, offering hope for improved perinatal outcomes.

