Fetal Tetralogy of Fallot (TOF) is the most common cyanotic congenital heart defect (≈1 in 3500 live births, 7–10% of CHDs). Prenatal TOF diagnosis prompts detailed counselling about prognosis. Modern management yields very high survival (>95%), but affected infants require at least one major surgery (complete intracardiac repair). A subset (∼20 %) may need a neonatal palliative shunt or ductal stent before complete repair. After successful repair, many patients eventually develop right ventricular outflow or pulmonary valve dysfunction requiring re-intervention. These facts inform our approach to counselling families early in pregnancy.
1. Early Fetal Period Assessment (before 24 weeks)
Why it matters:
- Families often base their decision not only on survival but also on the burden of future surgeries.
- In some countries like India, termination of pregnancy (MTP) is legally permissible till 24 weeks.
Fetal Echo Predictors for Duct Dependency or Neonatal/ Early Intervention:
- Pulmonary valve annulus Z score ≤ –3 (also associated with high reintervention rate)
- PV velocity ≥ 87.5 cm/s (Gradient ≈ 3mmHg) at 19–22 weeks (Escribano-Galindo et al.).
- Main PA <50% Ao size
- Poor PA growth trajectory already visible on serial scans.
- Rarely: progression to atresia (~6%) but needs to be mentioned.
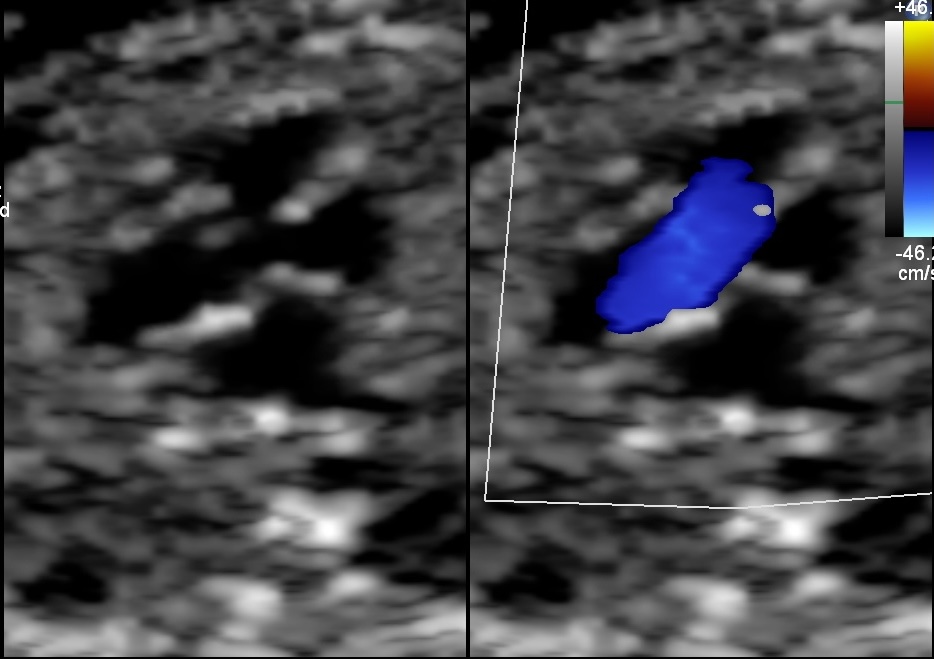

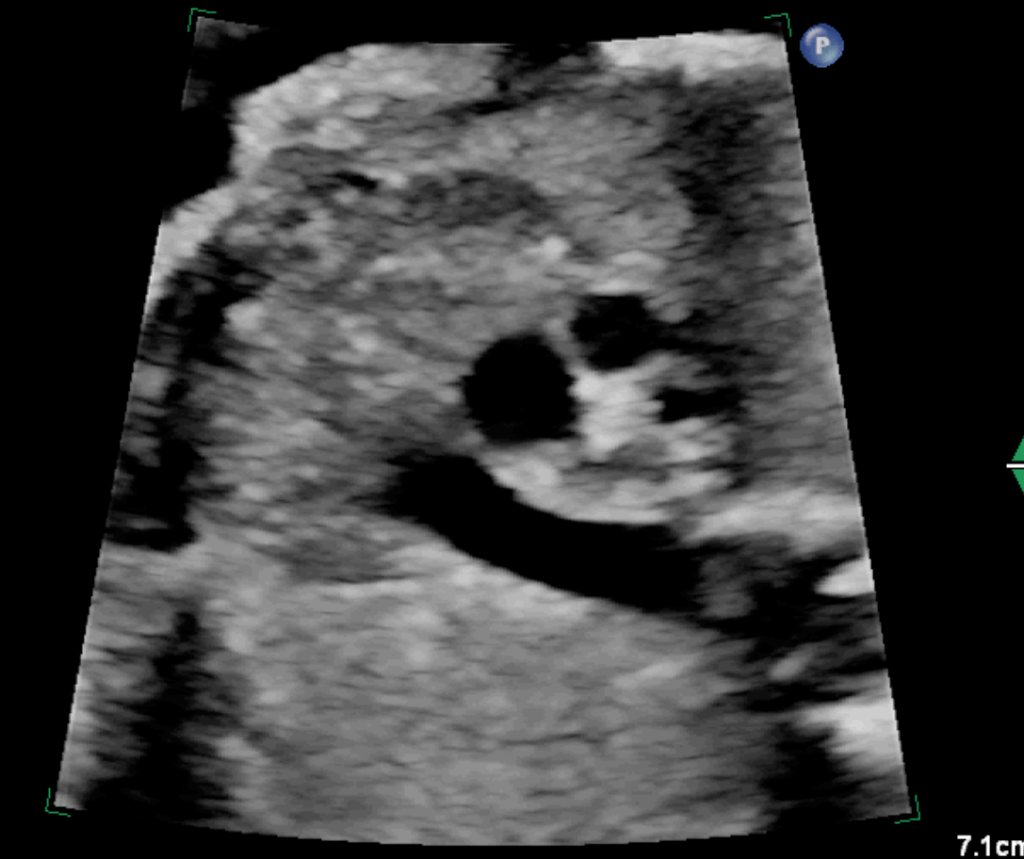
Image: Case of Fetal ToF with Right Aortic Arch with a significantly small pulmonary artery and a small Thymus. Dipicting high-risk features for the likelihood of the post-natal duct dependency and association with 22q11 deletion.
Counselling approach:
- If predictors are severe (ductal-dependent, multiple interventions likely), discuss the realistic burden of surgery.
- If anatomy is favourable (PV annulus not too small, PA growth reasonable, no reversed DA), survival is excellent, usually single complete repair in infancy, and a lesser possibility of reintervention.
- Parents must weigh surgical burden against long-term quality of life; in severe cases, continuation of pregnancy may be reconsidered after full counselling.
2. Late or Near-Term Assessment: >28-32 weeks for severity
Why it matters:
- At this stage, termination is generally not an option. Focus shifts to perinatal planning.
Fetal Echo Predictors for Duct Dependency or Neonatal/ Early Intervention:
- PV Z score ≤ –5 or
- PV Z score < –3 with reversed DA flow (Arya et al.; Vetten et al.)
- PV velocity >144 cm/s (Gradient ≈ 8mmHg) (Escribano-Galindo et al.)
- Main PA <50% Ao size
How to counsel:
- Emphasise delivery at a tertiary cardiac centre if ductal dependence or critical anatomy.
- Timing: Plan induction at 39 weeks, during the daytime, with the cardiac, NICU, and surgical teams alerted.
- Expected course:
- Stable TOF: observation, elective repair at 3–6 months or later.
- Ductal dependent: PGE infusion → early palliation (shunt/stent) → later repair.
Summary for Practice
18–24 weeks:
- Focus on long-term surgical burden.
- Use PV Z-score, PV velocity, and PA size to predict early reintervention.
- Offer genetic counselling (22q11).
- Families may opt to consider the option of discontinuing the pregnancy if multiple surgeries are likely.
Late gestation:
- Focus on safe delivery and early stabilisation.
- Use PV size, Doppler, DA flow, and absent PV features for planning.
- Counsel on immediate vs delayed repair expectations.
Conclusion
Prenatal diagnosis of TOF allows risk stratification and detailed counselling beyond the initial finding. Early (mid-trimester) fetal echocardiogram markers, especially small pulmonary valve size or high flow velocities, help predict which fetuses will be ductal-dependent or require neonatal intervention and higher possibility of reintervention after complete repair. Families should understand that, while survival is excellent, all children will undergo at least one surgery and often additional interventions. Genetic testing is essential due to the high rate of 22q11.2 deletions in TOF. In the later third trimester, multidisciplinary planning (including Obstetrics, Pediatric Cardiology, and Pediatric Cardiac Surgery) ensures that ductal-dependent infants receive immediate care at birth. In all cases, honest discussion of expected courses, from “one repair and good outcome” to “multi-stage palliation and frequent reinterventions”, enables parents to make informed decisions and prepares them for the neonatal period.

