Fetal Complete Heart Block (CHB) is often linked to connective tissue autoimmune disorders, such as Sjögren’s syndrome or systemic lupus erythematosus. Autoantibodies, particularly SSA/Ro and SSB/La, cross the placenta and affect the fetal cardiac tissue, notably the AV node. Interestingly, many of these women may be asymptomatic yet test positive for antibodies.
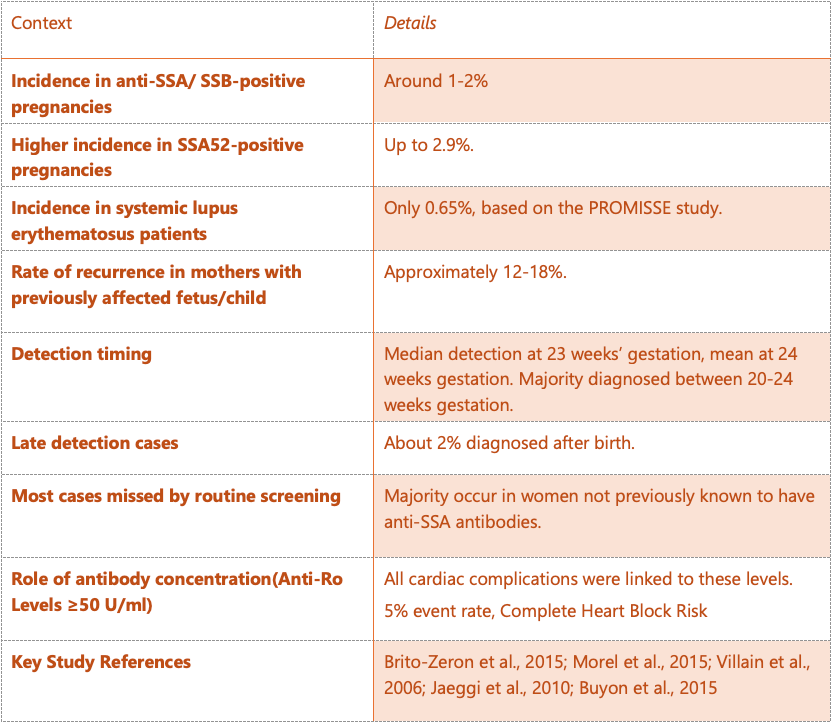
There are only 14 cases of La-mediated autoimmune complete heart block (CHB) in the published literature. Similar to Ro antibodies, serum levels of La antibodies are significantly higher in affected mothers compared to non-affected mothers. These cases represent less than 1% of known autoimmune CHB cases and should not be used as a biomarker to predict autoimmune CHB.
Pathogenesis
The pathogenesis of autoimmune chronic hepatitis B (CHB) involves the transplacental passage of maternal anti-SSA/Ro antibodies via the FcγRn receptor. These antibodies bind to the surface of apoptotic cardiomyocytes during fetal development, diverting the removal of these cells from a non-inflammatory pathway to one involving engulfment by macrophages. This process activates the TLR 7/8 cascade, leading to the production of pro-inflammatory and pro-fibrotic cytokines, such as TNF-α and TGF-β. An additional possible mechanism is that anti-Ro52 antibodies disrupt calcium homeostasis in cardiomyocytes, leading to intracellular calcium accumulation, loss of contractility, and cell death. Another theory is that upregulation of type I IFN in the mother with antibodies leads to direct stimulation of the inflammatory cascade. A second hit viral hypothesis is also proposed. These events culminate in inflammation, fibrosis, and eventual calcification of the cardiac system.
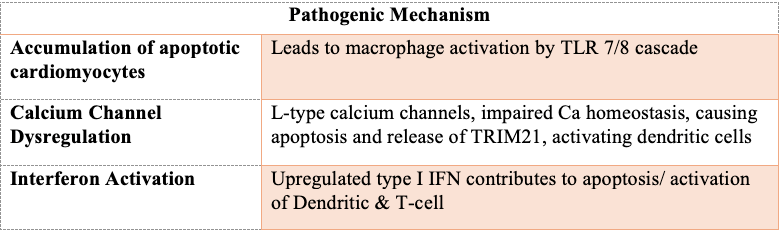
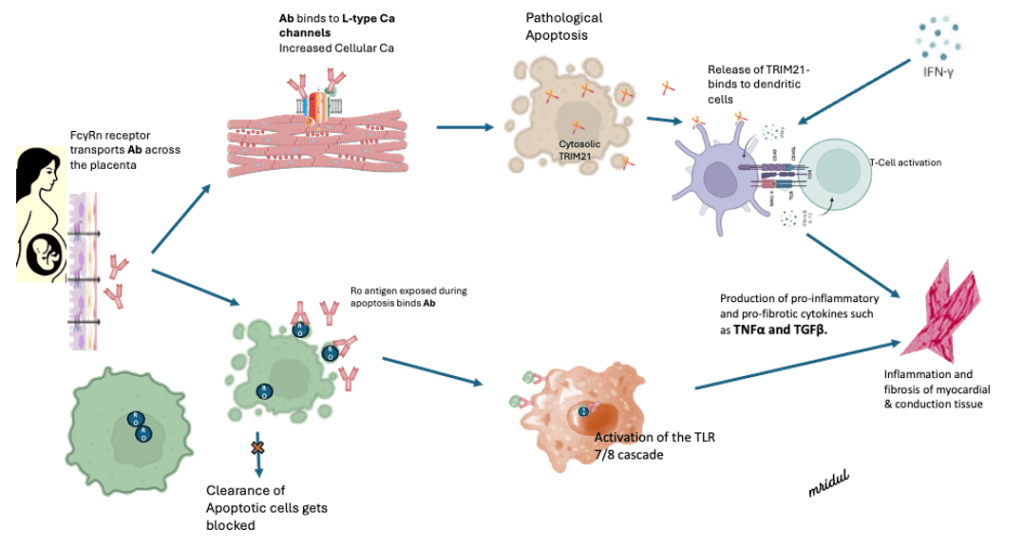
Cytokine response and secretion of proinflammatory mediators like TGF-β and TNF-α, promoting fibroblast differentiation and excessive scarring.
Monitoring
Monitoring the fetal rhythm in mothers with positive anti-Ro/La antibodies is currently recommended. Most centres adopt weekly or biweekly monitoring during high-risk periods and are more liberal during fringe periods. Some studies indicate that using a handheld Doppler for fetal heart rate and rhythm monitoring (FHRM) at home every 12 hours can improve outcomes. If an abnormality is detected, the patient receives an urgent fetal echo and treatment with dexamethasone and/or IVIG.

Treatment and Management
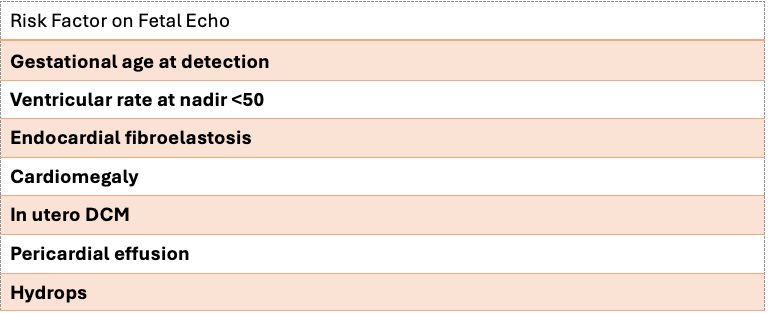
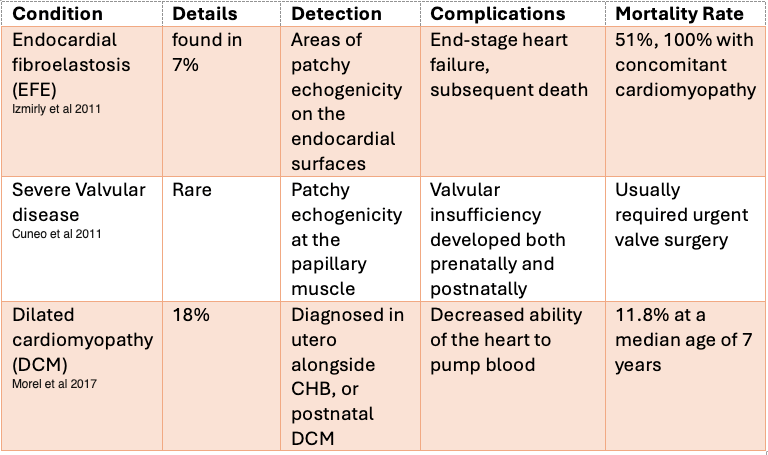
Untreated fetuses with isolated CHB have a perinatal mortality rate of up to 40%. Risk factors for adverse outcomes include fetal hydrops, endocardial fibroelastosis (EFE), a ventricular rate below 55 beats/min, and premature delivery. Antibody-mediated myocarditis, hepatitis, and dilated cardiomyopathy can also be diagnosed after birth in babies whose mothers have SLE. This forms the basis for treating fetuses with CHB to improve outcomes. However, concerns about the toxic effects of steroids on the developing fetus mean that treatment is not always an option.
Treatment Protocols
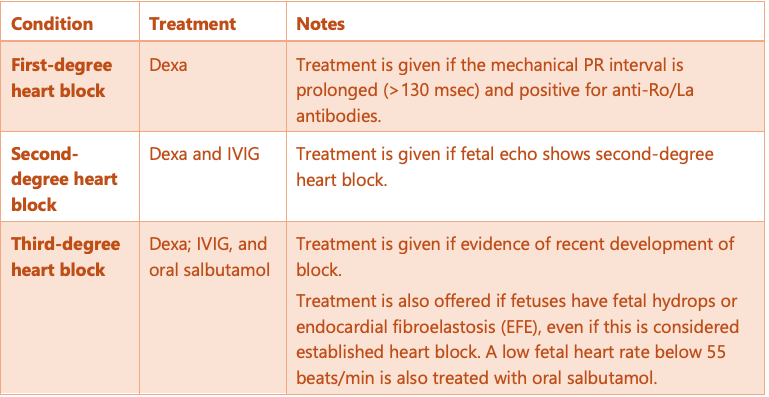
Treatment protocols vary between institutions. Initial studies suggested that Dex@meth@sone (Dexa) could improve first-degree heart block, but later studies showed similar outcomes with or without treatment. For second-degree heart block, Dexa and IVIG are commonly used, but the results can be variable. In cases of third-degree heart block, treatment is necessary for fetal hydrops, endocardial fibroelastosis (EFE), and low ventricular rates below 55 beats/min. However, the conduction is not expected to improve with treatment
Treatment Outcome
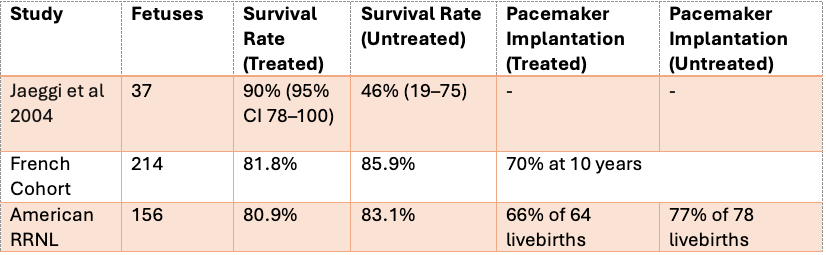
Among Fetal CHB, overall, 70% require a pacemaker by age 10, and the Mean 10-year survival rate is 86%
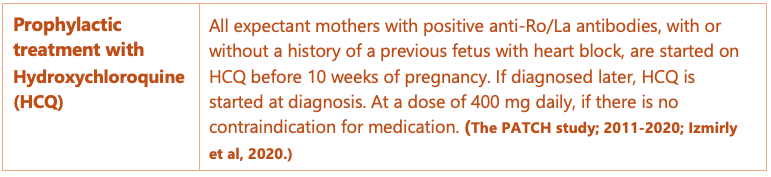
Prophylactic Treatment
Prophylactic treatment with Hydroxychloroquine (HCQ) has shown benefits in various studies. A recent study demonstrated a reduction in the recurrence of CHB by more than 50% with a daily dose of 400 mg of HCQ before the completion of the 10th gestational week and maintained throughout pregnancy.
Prognosis and Outcomes
The prognosis and outcomes for fetuses with isolated complete heart block largely depend on the pre›sence of fetal hydrops. Studies indicate that with isolated complete heart block, the Mortality rate is 17%-19%.
Cardiac Complications beyond Conduction Abnormality
How I manage it-
- HCQ Treatment: All expectant mothers with positive anti-Ro/La antibodies, with or without a history of a previous fetus with heart block, are started on HCQ before 10th week of pregnancy, or if diagnosed later, HCQ is started at diagnosis at a dose of 400 mg daily.
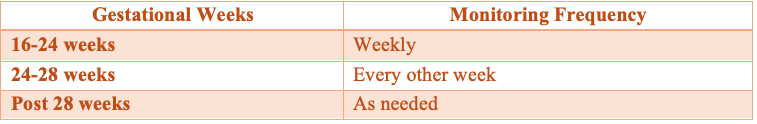
- Fetal Rhythm Monitoring: Weekly fetal rhythm monitoring is planned between 16-24 weeks and every other week until 28 weeks. Home Doppler rate monitoring is not currently included in our protocol.
- Mechanical PR Interval: The mechanical PR interval is assessed by the mitral-aorta pulsed-wave Doppler method during fetal echo. A duration of >130 msec is considered prolonged (+2 z score), and >150 msec (+3 z score) is considered a first-degree heart block. Mothers with prolonged PR intervals and positive anti-Ro/La antibodies are treated.
- Second-Degree Heart Block: If fetal echo shows a second-degree heart block, Dexa and IVIG treatment are given.
- Third-Degree Heart Block: If a fetal echo reveals a third-degree heart block, treatment is initiated if evidence of recent (within 7-10 days) development of complete heart block is noted, after explaining the possible benefits to the patient (shared decision-making). Treatment is also offered if fetuses have fetal hydrops or endocardial fibroelastosis (EFE), even if this is considered established heart block. A low fetal heart rate below 55 beats per minute is also treated with oral salbutamol.
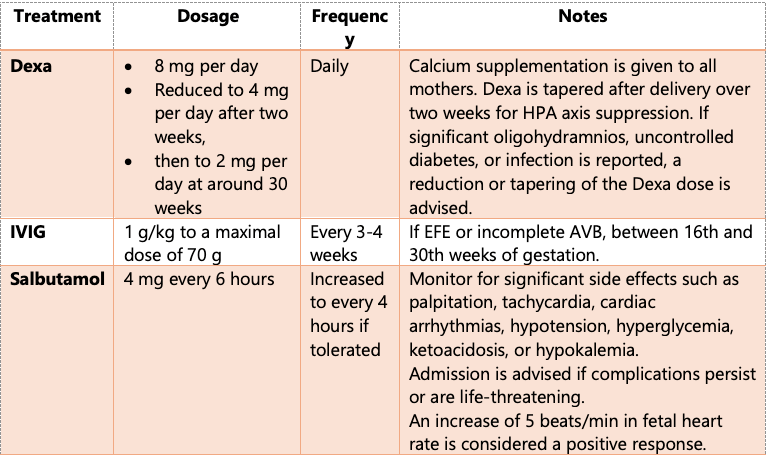
- Dex@meth@sone: is started at 8 mg per day, reduced to 4 mg per day after two weeks, and then to 2 mg per day at around 30 gestational weeks. Calcium supplementation is given to all mothers. Precautions to avoid gastritis are taken. Dexa is tapered after delivery over two weeks for HPA axis suppression. If significant oligohydramnios, uncontrolled diabetes, or infection is reported, a reduction or tapering of the dose is advised.
- IVIG: IVIG is usually administered four times at a dosage of 1 g/kg 1 g/kg to a maximal dose of 70 g, every 3-4 weeks, between the 16th and 30th weeks of gestation.
- Salbutamol: Salbutamol is started at a dose of 4 mg every 6 hours and increased to every 4 hours if tolerated. In case of significant palpitation, tachycardia, cardiac arrhythmias, hypotension, hyperglycemia, ketoacidosis, or hypokalemia, admission is advised, and the dose is decreased if complications persist or are life-threatening. A 5-beat/min increase in fetal heart rate is considered a positive response.
Conclusion
Immune Heart Block is partially preventable and potentially treatable if detected early. Frequent check-ups are desirable but can be limited by practical constraints. Treatment guidelines are evolving, with variable outcomes reported for Dexa, hydroxychloroquine (HCQ), and intravenous immunoglobulin (IVIG) treatments. Clinical judgment, along with open discussions between caregivers and families, is essential in planning the management strategy and in clarifying expectations regarding prognosis and outcomes.