Fetal heart rate (FHR) is a cornerstone in prenatal monitoring. Traditionally, obstetric ranges have been utilized to evaluate fetal well-being and fetoplacental adequacy. However, integrating gestational age-specific ranges offers an additional perspective in fetal cardiac monitoring, helping to predict rare, life-threatening conditions that can present as a low baseline heart rate for gestational age. This blog post explores the value of gestational FHR ranges and the distinct roles of obstetric and gestational ranges in prenatal care.
Obstetric Fetal Heart Rate Range: A Snapshot for Acute Management
The obstetric FHR range, spanning 110 to 160 beats per minute (bpm), is crucial for assessing fetal well-being, fetal distress during labor, and acute fetoplacental insufficiency episodes. An FHR of less than 110 bpm indicates potential fetal compromise. This range is a quick reference for managing peripartum emergencies and ensuring fetal stability and placental sufficiency.
Gestational Fetal Heart Rate Range: A Tool for Screening beyond fetal well-being.
Gestational age-specific FHR percentiles (<3rd to >97th percentile) are based on FHR measurements in normal, uneventful pregnancies. These ranges provide critical insights into fetal development and help detect abnormalities.
- Gestational Bradycardia:
- FHR below the 3rd percentile for gestational age (GA) is termed gestational bradycardia.
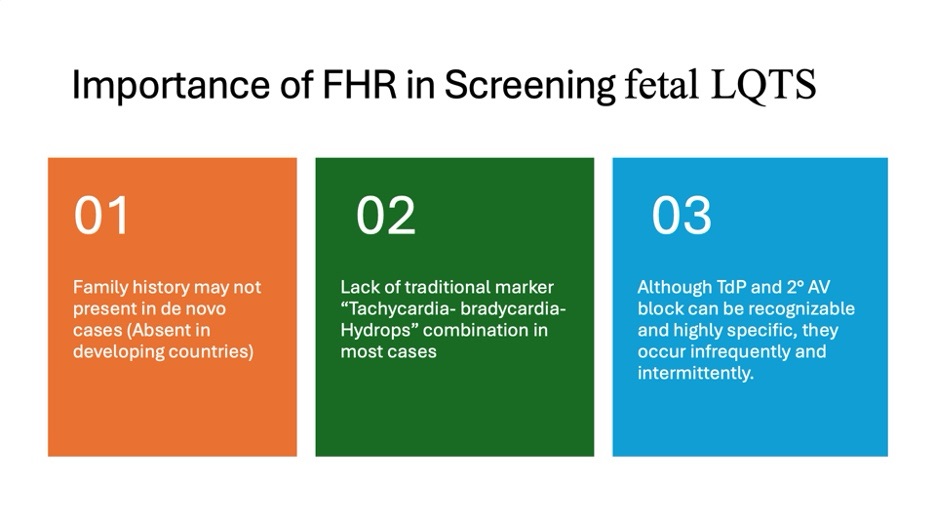
- Persistent low baseline FHR below gestational cutoffs enhances the ability to detect subtle signs of channelopathies, such as sinus bradycardia due to conduction abnormalities or sympathetic imbalances, which may progress over time.
A study by Mitchell et al. established gestational FHR norms in normal fetuses and evaluated baseline FHR in fetuses with long QT syndrome (LQTS).
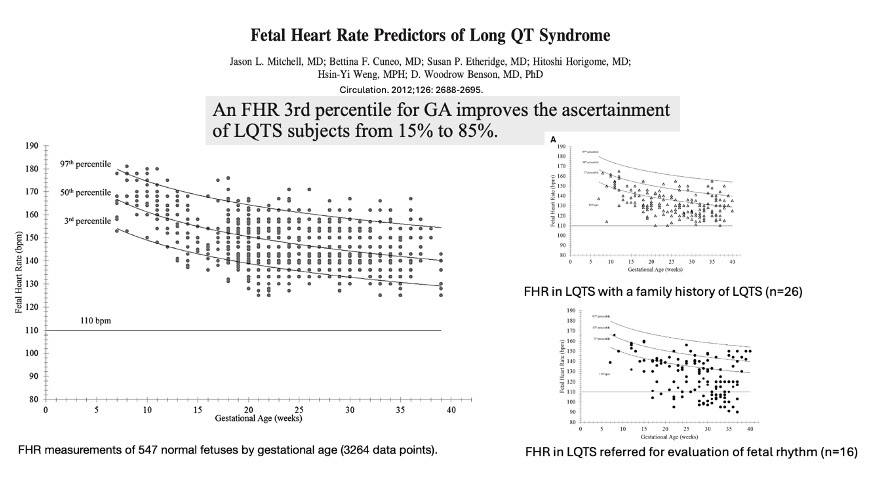
Similarly, Cuneo BF et al. demonstrated that 85% of LQTS cases (11 out of 13) could have been missed without GA-specific FHR norms.
Beyond LQTS: Insights Into Genetic Variants
- RYR2 and HCN4 Gene Variants:
- These are associated with distinct FHR profiles and structural anomalies, such as ventricular septal defects and outflow tract anomalies.
- Fetuses with the HCN4 mutation typically present with sinus bradycardia, ventricular non-compaction, and structural defects, including ventricular septal and outflow tract anomalies. These mutations carry a lower risk of sudden death but a higher likelihood of extranodal disease.
- Importance of Recognizing Low FHR:
- Increased recognition of low FHR is vital for evaluating other causes of sinus bradycardia and guiding appropriate interventions.
Clinical Implications
Adopting gestational FHR ranges allows for:
- Improved Detection: Earlier recognition of conditions like LQTS.
- Personalized Care: Tailoring interventions based on genetic insights and longitudinal data.
Importance of Prenatal Diagnosis of LQTS
- Pregnancy can be risk-stratified to provide targeted care.
- Effective in-utero treatment of ventricular tachycardia (VT) has prolonged gestation and resolved fetal hydrops.
- Fetuses with suspected fetal distress due to sinus bradycardia are not delivered urgently or prematurely if the bradycardia is recognized as attributable to the LQTS phenotype.
- Primary prevention of malignant arrhythmias is highly effective in LQTS.
- Cascade genetic screening offers significant benefits for family members.
Complementary Roles of Obstetric and Gestational FHR Ranges
- Obstetric Ranges: Best suited for acute monitoring of fetal well-being, especially during labor and detecting prepartum distress. The presence of FHR less than 110/min needs action to manage the fetus’s well-being.
- Gestational Ranges: Essential for identifying true sinus bradycardia, identifying genetic abnormalities, and guiding long-term management. The presence of low baseline fetal heart rate necessitates further evaluation.
Conclusion
Fetal heart rate monitoring is a dynamic tool in prenatal care. Leveraging obstetric and gestational FHR ranges ensures a comprehensive assessment, balancing immediate fetal well-being with long-term developmental insights. A persistent fetal heart rate below the gestational 3rd percentile should never be left without further evaluation for genetic channelopathies, especially LQTS. Integrating these approaches strengthens collaboration between obstetrics and pediatric cardiology, optimizing outcomes for both mother and fetus.

