Introduction
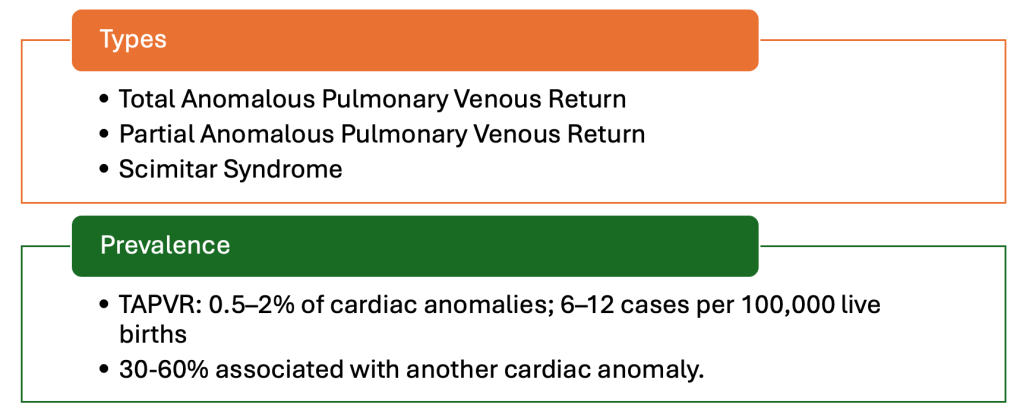
Total anomalous pulmonary venous connection (TAPVC) is a rare but critical congenital heart anomaly where the pulmonary veins fail to connect to the left atrium. Early and accurate prenatal diagnosis is vital for optimizing postnatal outcomes.
Understanding TAPVC in Fetal Cardiology
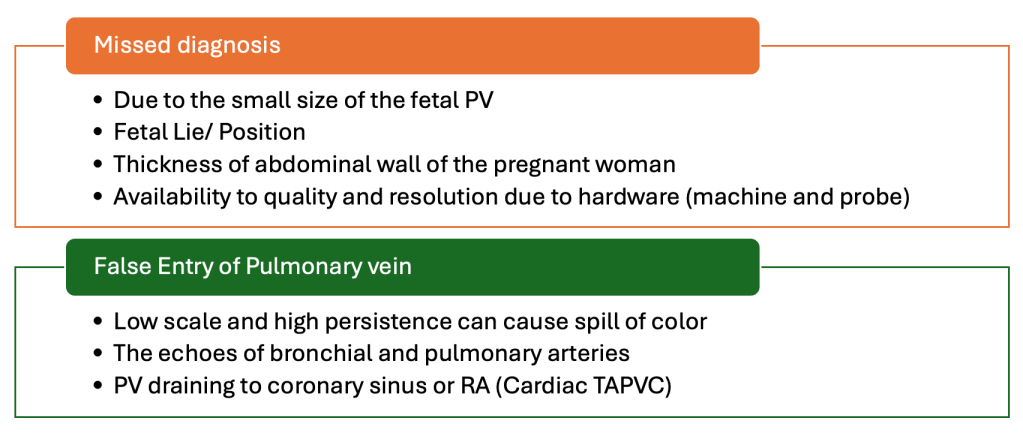
TAPVC often poses diagnostic challenges due to subtle findings during routine fetal echocardiography. Despite advances in imaging, detection rates remain modest, ranging from 8% to 50% in various studies. Here’s how to enhance diagnostic accuracy.
Key Diagnostic Markers
Absence of Pulmonary Veins in the Left Atrium (LA)
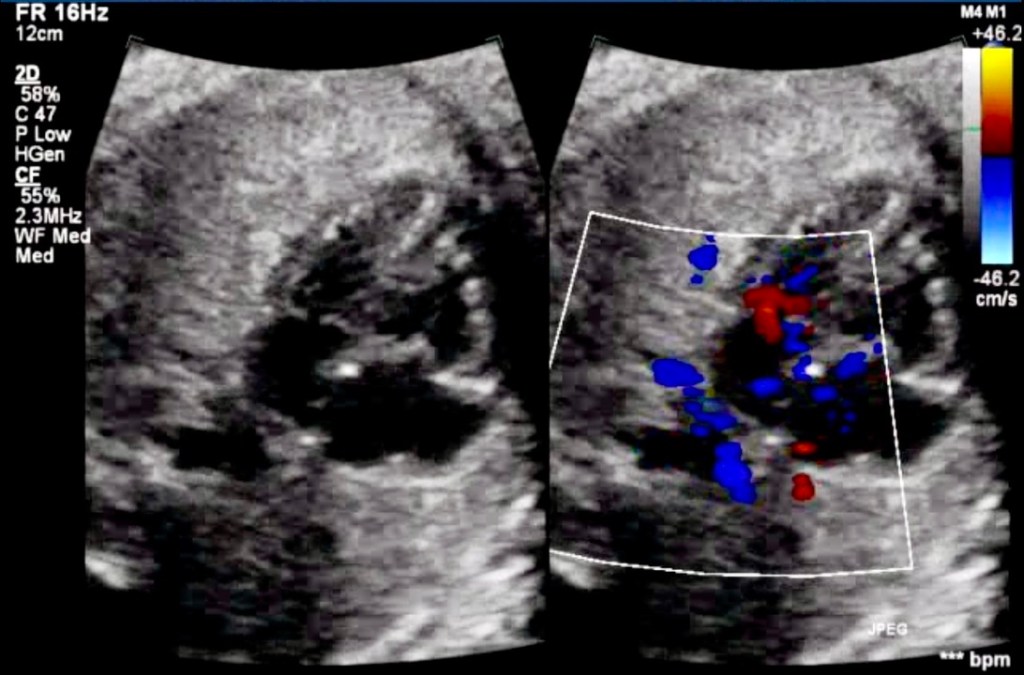
A definitive marker of TAPVC is the lack of pulmonary venous entry into the LA. This hallmark finding can be overlooked without systematically examining pulmonary venous connections.
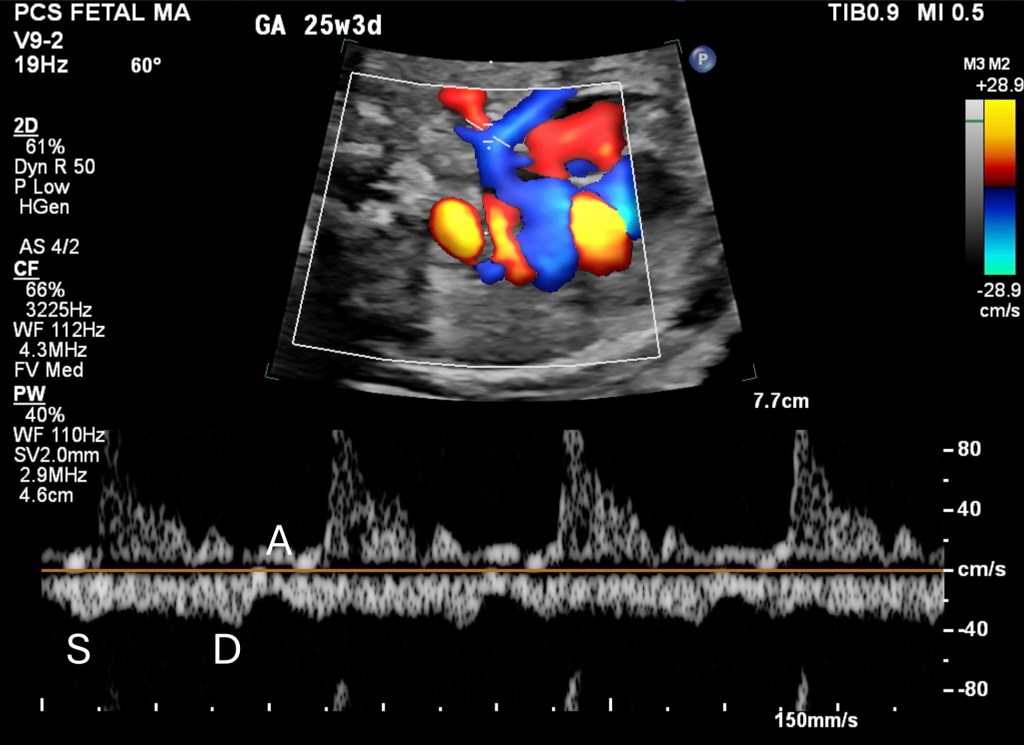
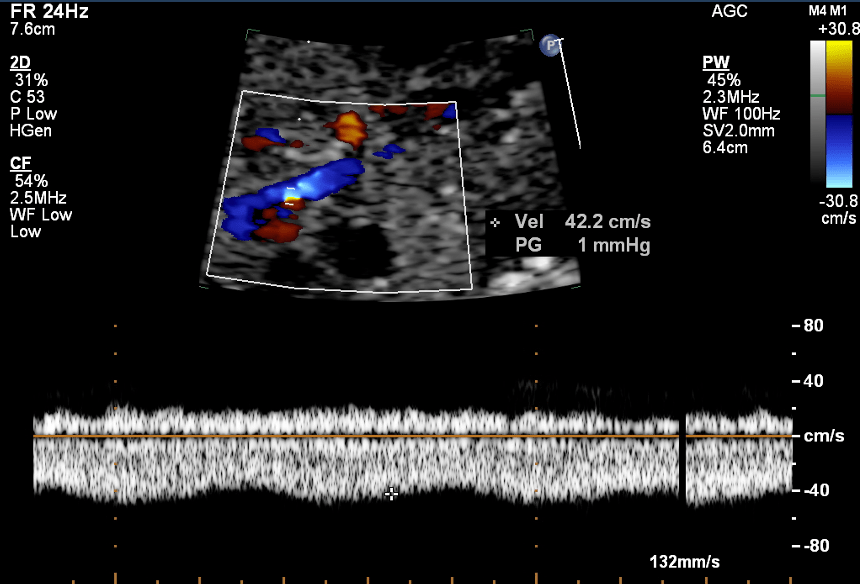
Pulmonary Venous Doppler Patterns
- Doppler waveforms provide critical diagnostic support, and confirmation.
- Biphasic waveforms with reduced pulsatility or abnormal monophasic flow patterns are typical in TAPVC.
Subtle Indicators / Screening Marker
Ventricular Disproportion
An enlarged right ventricle relative to the left may reflect increased systemic flow, often seen in TAPVC.

Paladin et al. 2017 cohort study found it in 59.2% of cases for an LV/RV of >0.66 (or RV/LV of 1.5).
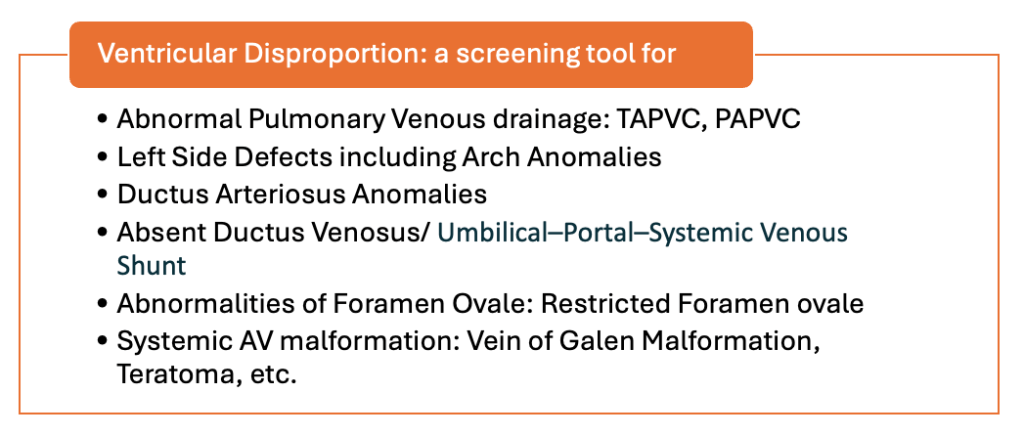
More about Ventricle Disproportion
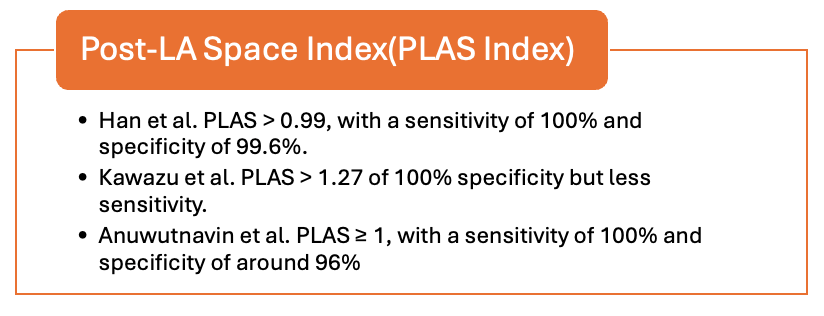
Post-LA Space Index
This index measures the distance between the LA and descending aorta, with higher values suggesting TAPVC. Studies show remarkable sensitivity and specificity with this method.
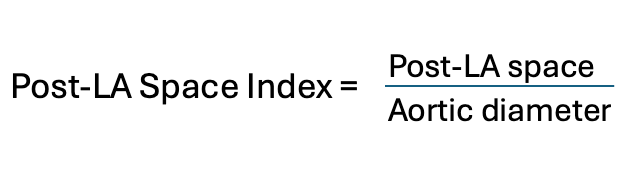
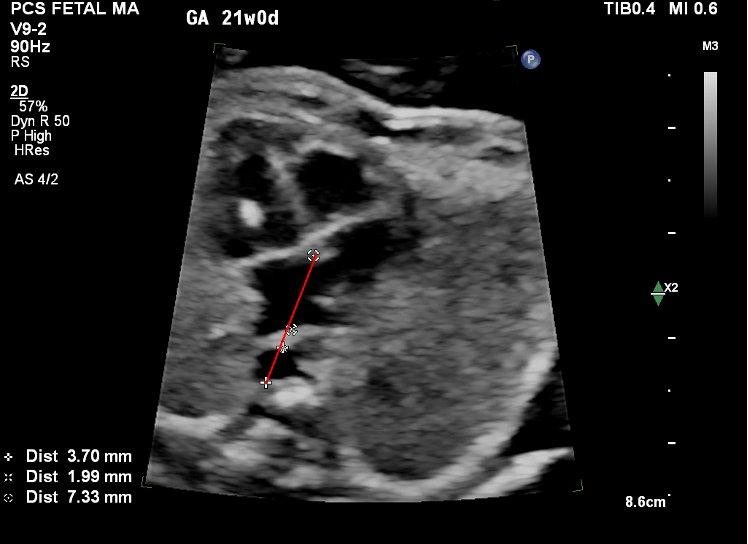
Measurement should be made in the line connecting the DTA diameter with the crux of the heart.
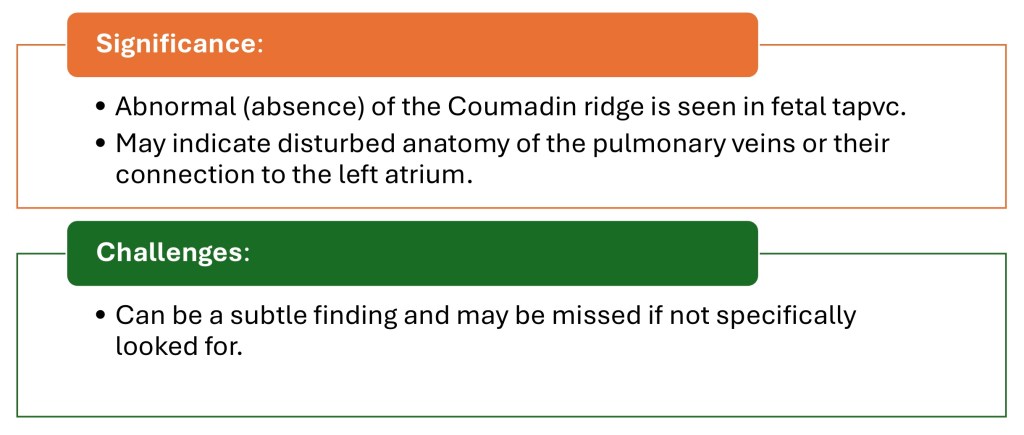
Absent Coumadin Ridge
The absence of this structure, which separates the left upper pulmonary vein from the left atrial appendage, points to abnormal pulmonary venous anatomy.
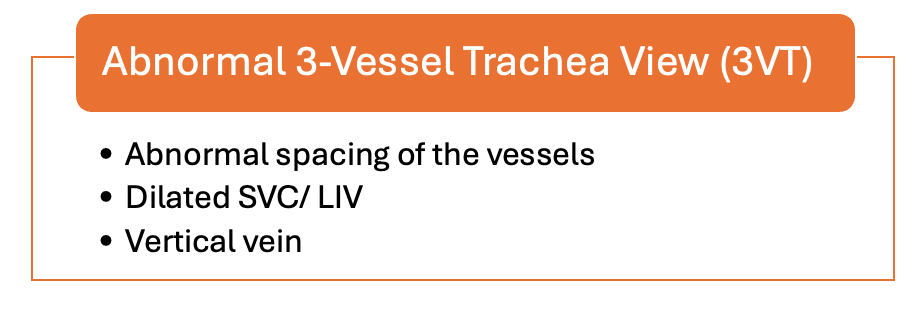
Three-Vessel View (3VV)
Smooth Posterior Wall of LA
- The posterior wall of the LA typically appears irregular due to pulmonary vein entry points. A smooth posterior wall raises suspicion.
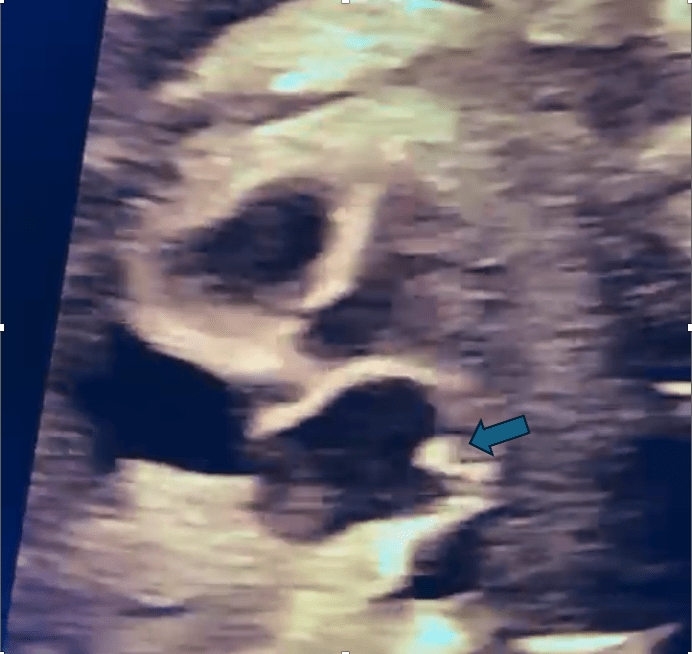
Presence of a Confluence Behind the LA (Twig Sign)
- Identifying a venous confluence posterior to the LA is a vital clue. The absence of a normal Coumadin ridge can complement this.
Why Early Diagnosis Matters
Prenatal identification of TAPVC allows for:
- Timely planning of delivery at a tertiary care center.
- Multidisciplinary coordination for immediate postnatal stabilization and surgery.
Take-Home Algorithm for TAPVC Screening
- Initial Screening Views: Use the 4-chamber to track drainage of pulmonary veins, 3VV, and 3VT views.
- Identify Soft Markers: Look for ventricular disproportion, Post-LA Space Index, a smooth LA posterior wall, or an abnormal Doppler pattern.
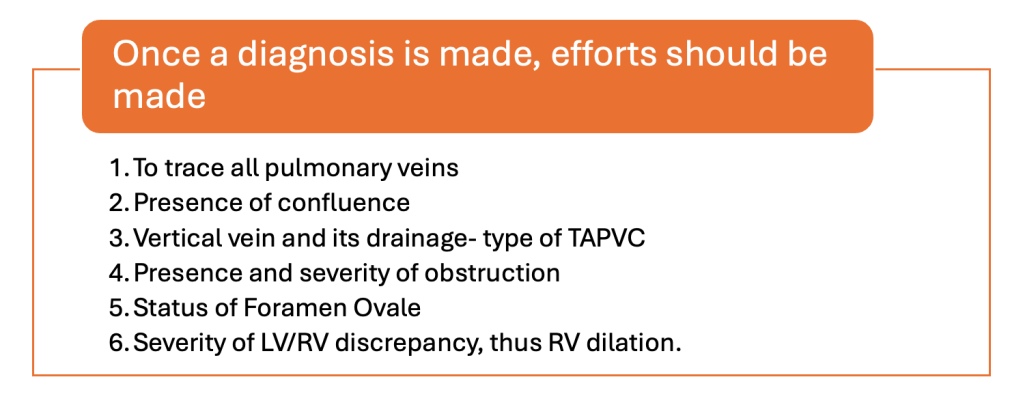
- Confirmatory Imaging: To solidify the diagnosis, track all pulmonary veins, venous confluence, vertical vain, and grade obstruction.

Conclusion
Detecting fetal TAPVC requires a keen eye and systematic evaluation during fetal echocardiography. By recognizing key markers and incorporating advanced imaging techniques, obstetricians and fetal medicine specialists can significantly improve diagnostic rates and outcomes for these high-risk pregnancies.

