
For fetal monitoring, particularly in high-risk pregnancies, two key scores have emerged as vital tools for assessing fetal well-being: the Fetal Cardiovascular Profile Score (CVPS) and the Cerebro-Placental Ratio (CPR). Each score offers unique insights into the fetus’s cardiovascular health and its ability to cope with stressors like placental insufficiency, intrauterine growth restriction (IUGR), and fetal distress. Understanding how these two assessments work together can significantly enhance the management of pregnancies where fetal health is in jeopardy.
The Fetal Cardiovascular Profile Score (CVPS): A Comprehensive Assessment of Heart Health
The CVPS evaluates various aspects of fetal cardiovascular function, combining multiple parameters into a single score to offer a holistic view of the fetus’s health.
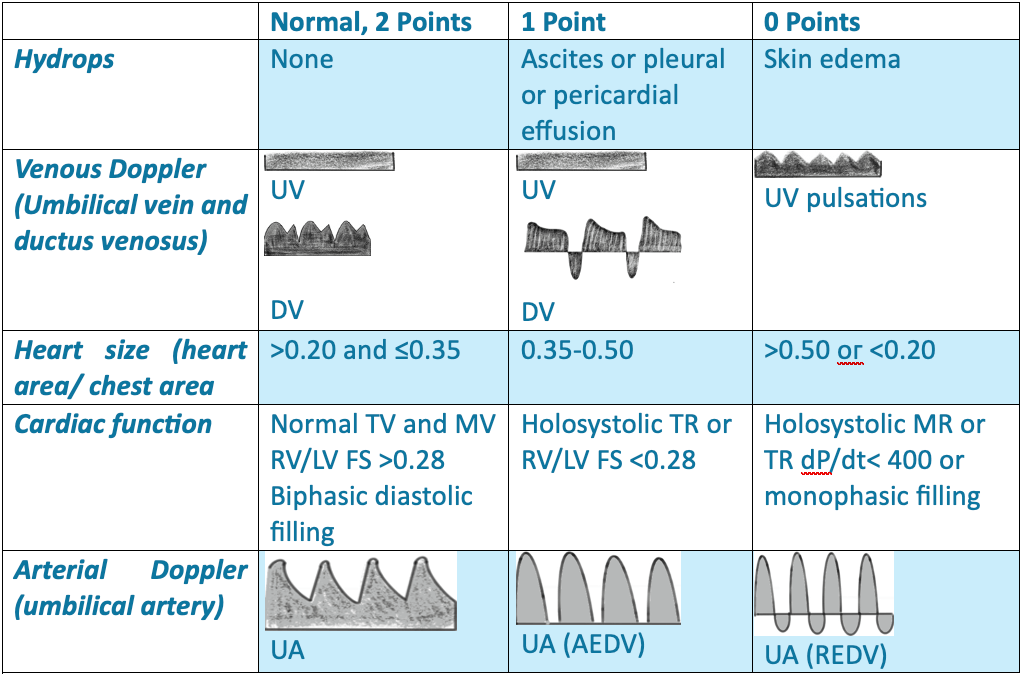
CVPS Scoring Interpretation:
Fetal Heart Failure (FHF) severity is assessed using a 10-point scale, where a score of 10 indicates the absence of heart failure. Points are subtracted based on abnormalities in each component marker.
- 10 points: Normal
- 9-8 points: Mild heart failure, likely compensation for any placental insufficiency. These fetuses generally do not require immediate delivery, but ongoing monitoring is essential.
- 6-7 points: Moderate Heart Failure, (Mild Fetal Distress): Indicates early signs of fetal compromise, warranting closer surveillance. This may suggest moderate placental insufficiency or early-stage fetal heart dysfunction.
- < 5 points: Severe Heart Failure, (Severe Fetal Distress): Signifies significant cardiovascular compromise and potential heart failure. Immediate delivery is often considered to prevent fetal demise.
Clinical Application of CVPS in IUGR and Fetal Distress:
The CVPS provides a comprehensive picture of fetal cardiovascular function and helps guide management in cases of IUGR and fetal distress:
- Serial Assessments: By tracking CVPS over time, clinicians can monitor the progression of fetal compromise. A declining score often indicates worsening fetal condition, prompting intervention.
- Decision for Delivery: A low CVPS (< 6), especially when combined with abnormal Doppler findings (e.g., reversed A-wave in the ductus venosus), suggests that immediate delivery should be considered, even if the fetus is preterm.
- Complementary to Doppler Studies: The CVPS integrates the results of Doppler studies (e.g., ductus venosus A-wave) with other clinical parameters, providing a more holistic assessment of fetal health compared to Doppler indices alone.
- Monitoring Over Time: Serial CVPS assessments allow for tracking the progression of fetal compromise, helping clinicians decide when continued monitoring is safe versus when urgent intervention is needed.
Cerebro-Placental Ratio (CPR): Understanding Blood Flow Redistribution
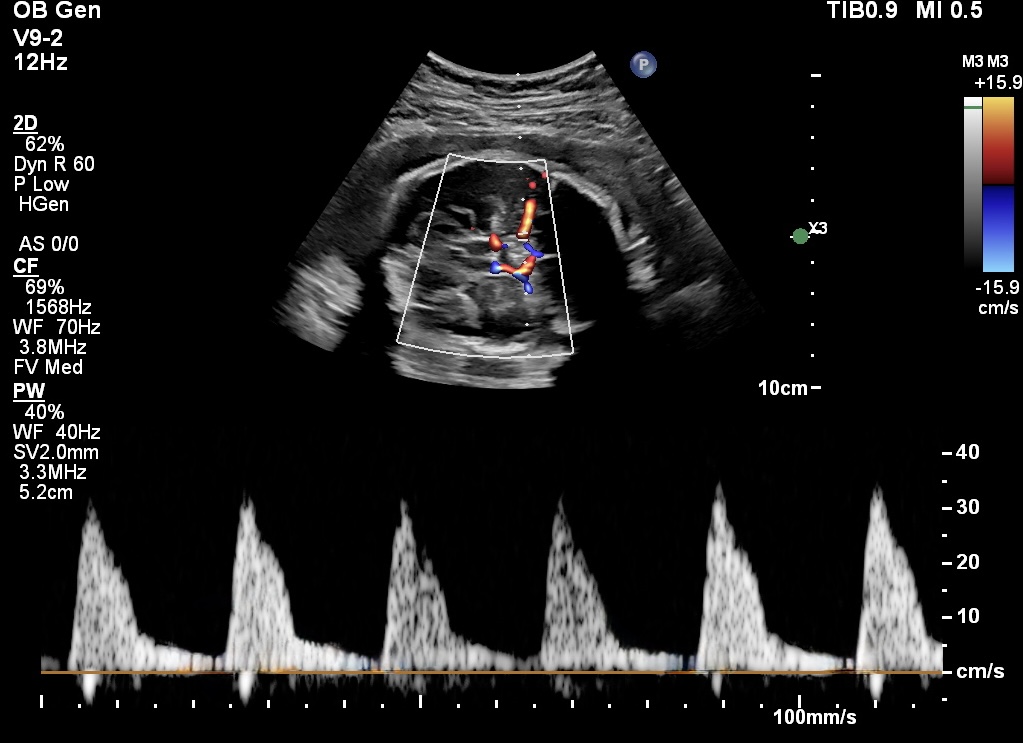
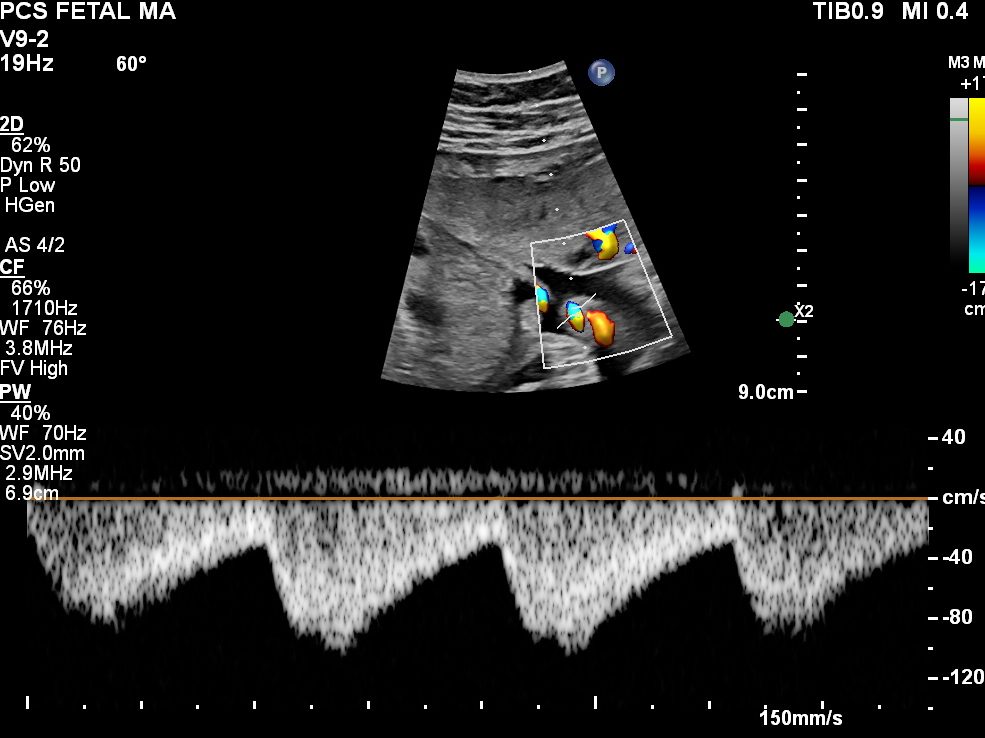
The Cerebro-Placental Ratio (CPR) is calculated by comparing the blood flow in the middle cerebral artery (MCA) to the umbilical artery (UA), giving clinicians a clear understanding of the fetus’s brain-sparing effect—the ability to redirect blood to vital organs like the brain when placental blood flow is insufficient.
It is calculated as the ratio between the pulsatility index (PI) of the middle cerebral artery (MCA) and the pulsatility index (PI) of the umbilical artery (UA).
CPR=PI-MCA/ PI-UA
CPR and Fetal Well-Being:
Normal CPR (1.5-2.0): Indicates normal fetal circulation with appropriate oxygen distribution between the placenta and brain. Fetuses with normal CPR are usually in good health, and their placental function is adequate.
Low CPR (< 1.0): Suggests the fetus is compensating for placental insufficiency by redistributing blood flow to the brain. This is an early sign of IUGR, and if uncorrected, may progress to fetal distress.
Declining CPR Over Time: A declining CPR indicates worsening placental function and fetal adaptation, often requiring closer monitoring, and possibly early delivery if other signs of fetal distress appear.
When to Act on CPR Findings:
Mildly Low CPR (0.8–1.0): May warrant increased surveillance, particularly if the pregnancy is complicated by IUGR, pre-eclampsia, or other risk factors.
Severely Low CPR (< 0.8): Indicates more severe fetal compromise and is often a marker for urgent delivery if other signs of fetal distress are present (e.g., abnormal ductus venosus Doppler, oligohydramnios).
Clinical Significance of Low CPR:
Fetal Adaptation to Hypoxia: A low CPR reflects the fetus’s adaptation to chronic hypoxia due to placental insufficiency, where blood is redirected to vital organs such as the brain to ensure survival.
Indicator of IUGR: A low CPR is often associated with Intrauterine Growth Restriction (IUGR). This compensatory mechanism can occur even before significant changes are seen in the fetal biometry or other Doppler indices.
CVPS and CPR: Complementary Tools for Fetal Well-Being
Both the CVPS and CPR provide unique but complementary insights into fetal well-being. While the CVPS offers a comprehensive assessment of cardiovascular function and the risk of heart failure, the CPR focuses on blood flow redistribution and the fetus’s ability to compensate for placental insufficiency.
How CVPS and CPR Work Together:
Early Warning Signs: CPR is often one of the first indicators of fetal adaptation to stress. A declining CPR suggests that the fetus is under stress, even if the CVPS remains stable. As the fetus continues to compensate, a low CPR may eventually be followed by a drop in CVPS, signaling a more urgent need for intervention.
Comprehensive Monitoring: CVPS and CPR provide a more complete picture of fetal health than either score alone. The CVPS evaluates the heart’s ability to cope with increased demands, while the CPR assesses how the circulatory system adapts to placental insufficiency.
Timing and Decision-Making: These scores help clinicians determine when to intervene in clinical practice. For example, a fetus with a low CPR but a stable CVPS may still be closely monitored without immediate delivery, but if both scores begin to decline, this often indicates a need for urgent action to avoid fetal demise.
Conclusion: The Tale of Two Scores
In the current era of fetal medicine, both the CVPS and the CPR play crucial roles in ensuring the best outcomes for high-risk pregnancies. The CVPS offers a comprehensive cardiovascular assessment, while the CPR gives insight into how well the fetus is compensating for placental issues. When used together, these two scores provide clinicians with a powerful toolset to monitor fetal health, optimize the timing of delivery, and improve perinatal outcomes.
By understanding and utilizing both the CVPS and CPR, clinicians can better navigate the complex challenges of fetal distress, IUGR, and other high-risk conditions, ensuring a safer pathway to delivery and a healthier start to life for vulnerable fetuses.
