
The Ductus Venosus (DV) serves as a pivotal channel in fetal circulation, diverting oxygen-rich blood from the umbilical vein directly to the inferior vena cava, thereby bypassing the liver.
This article provides a comprehensive guide to Doppler waveform analysis of the ductus venosus, emphasizing its significance in monitoring fetal health, particularly in high-risk pregnancies.
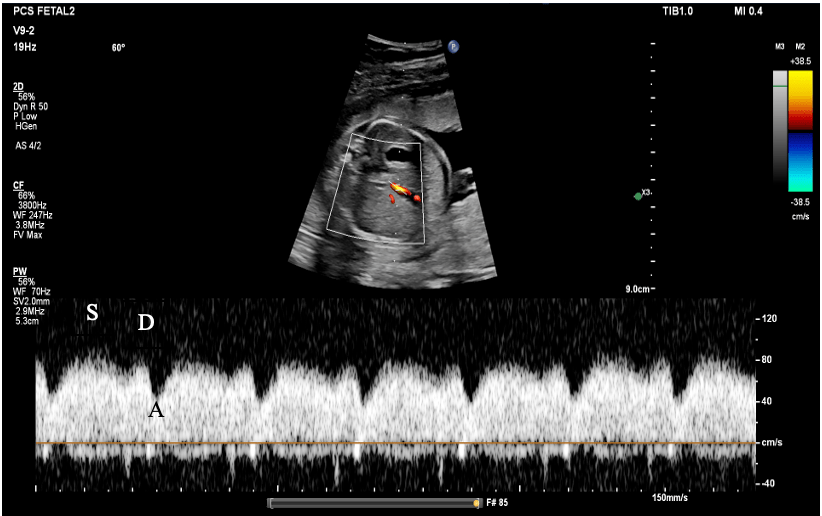
Understanding the Ductus Venosus Waveform The analysis of the Doppler waveform of the ductus venosus reveals three crucial phases:
- S-wave (Systole): This represents forward flow during ventricular systole, highlighting the peak positive wave as the heart contracts.
- D-wave (Diastole): Occurring during early diastole as the ventricles relax, this wave indicates forward flow with a magnitude typically smaller than the S-wave.
- A-wave (Atrial Contraction): This crucial wave denotes forward flow during atrial contraction, illustrating the pressure differential between the right atrium and the ductus venosus.
Normal Ductus Venosus Waveform Characteristics in the Second Trimester The second trimester is a critical period for fetal monitoring via DV analysis:
- S-wave: Notably prominent and positive.
- D-wave: Positive, though generally smaller than the S-wave.
- A-wave: Maintains a position above the baseline, indicating healthy atrial contraction and an adequate pressure gradient.
3. Doppler Indices:
1. Pulsatility Index (PI):
The Pulsatility Index (PI) is a measure of the variability in blood flow velocity within a cardiac cycle.
PI=Vmax−Vmin/ Vmean
2. Resistance Index (RI):
The Resistance Index (RI) is a reflection of the resistance to blood flow within a vessel.
RI=Vmax−Vmin / Vmax
3. Peak Velocity Index for Veins (PVIV):
The Peak Velocity Index for Veins (PVIV) is a measure used specifically for venous blood flow, like in the ductus venosus.
PVIV=Vmax / Vmean
- Vₘₐₓ: Peak systolic velocity (maximum velocity during systole).
- Vₘᵢₙ: End-diastolic velocity (minimum velocity during diastole).
- Vₘₑₐₙ: Mean velocity over the cardiac cycle.
4. Normal Values in the Second Trimester:
- Peak Velocity Index for Veins (PVIV): This is an index used to assess the flow in the ductus venosus. A normal PVIV is typically around 1.0 to 1.2.
- Pulsatility Index (PI): Reflects the pulsatility of blood flow. A normal PI for the ductus venosus ranges from 0.60 to 1.20 in the second trimester.
- Resistance Index (RI): Normal RI values typically range between 0.6 and 0.8 in the second trimester.
- A-wave Presence: The A-wave should be positive; a normal waveform does not have a reversal or absence of the A-wave.
- S/A ratio: Second Trimester, the normal S/A ratio typically ranges from 2.5 to 3.5.
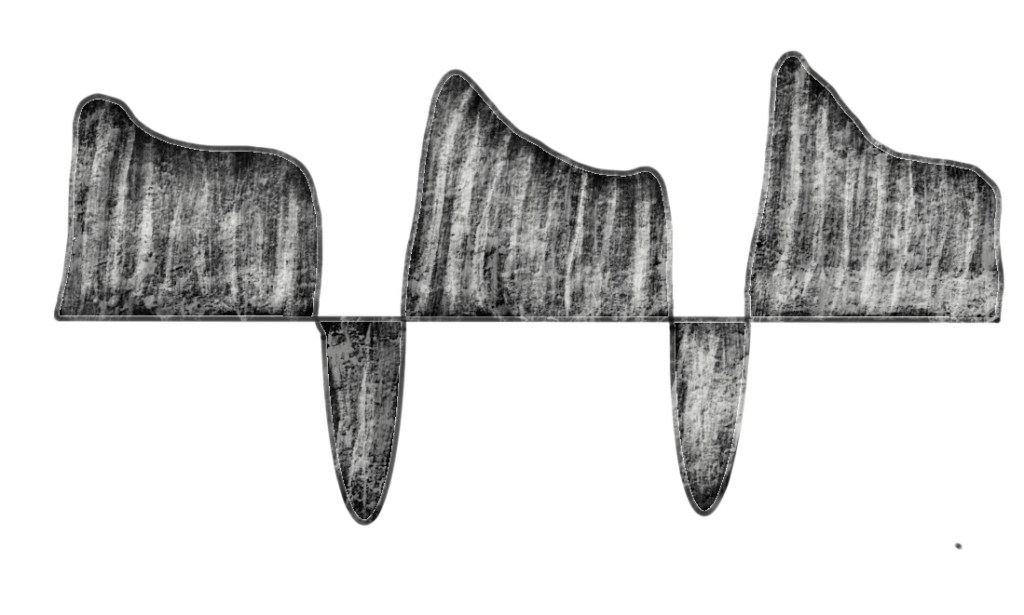
5. Abnormal Waveform Patterns and Clinical Significance:
- Absent or Reversed A-wave:
- Clinical Significance: This is a key indicator of increased right atrial pressure and potential fetal cardiac dysfunction. It is often associated with:
- Fetal Growth Restriction (IUGR): A reversed or absent A-wave is commonly seen in fetuses with severe IUGR, particularly if the condition is associated with placental insufficiency.
- Increased Risk of Fetal Demise: This waveform pattern is linked to poor perinatal outcomes, including stillbirth.

- Trisomy 21 and other aneuploidies: An abnormal ductus venosus waveform is often an early marker for chromosomal abnormalities.
- Cardiac Defects: Structural heart defects may also alter the normal waveform.
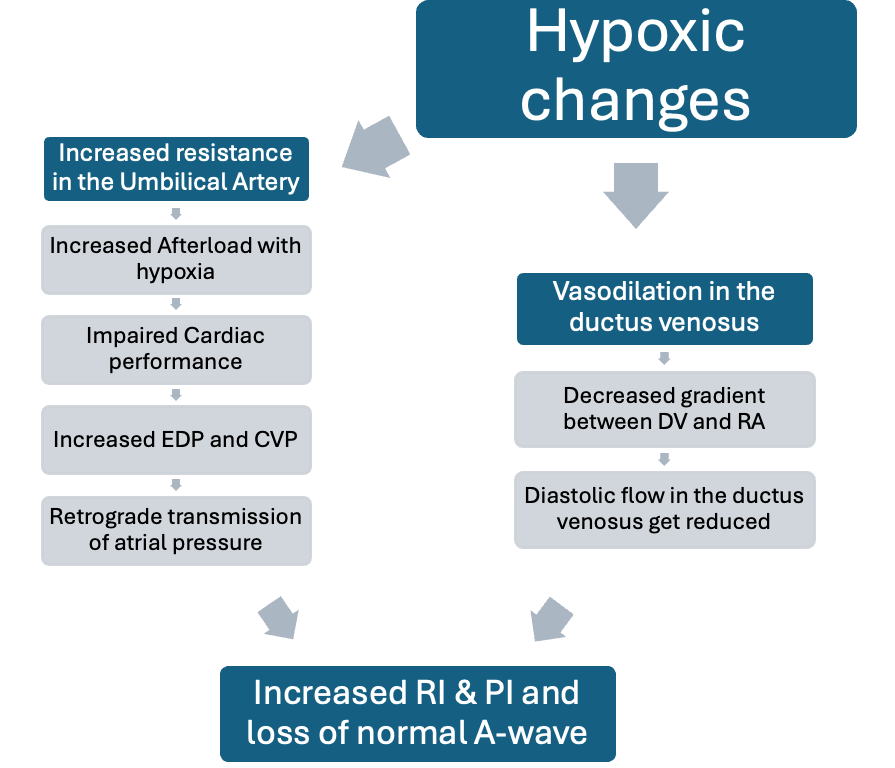
- Increased Pulsatility Index (PI):
- Clinical Significance: An increased PI suggests higher resistance to blood flow, often due to placental insufficiency. It can be an early sign of fetal compromise in conditions like pre-eclampsia and IUGR.
- Decreased D-wave:
- Clinical Significance: This can show poor diastolic function or elevated right ventricular pressures, both of which can be seen in fetuses with cardiac or systemic issues.
6. Clinical Applications:
- Monitoring IUGR: In cases of IUGR, serial ductus venosus Doppler studies help in monitoring fetal well-being and deciding the timing of delivery. An abnormal waveform is often a late sign and may prompt early delivery.
- Assessment of Cardiac Function: A ductus venosus waveform is a valuable tool in assessing fetal cardiac function, particularly in fetuses at risk for heart failure or those with known cardiac anomalies.
- Aneuploidy Screening: Abnormal ductus venosus waveforms, particularly during the first and second trimesters, are used as markers in combined screening protocols for aneuploidies, including trisomy 21.
7. Integration with Other Doppler Studies:
- Umbilical Artery Doppler: When combined with ductus venosus Doppler, it provides a comprehensive assessment of placental function and fetal circulatory adaptation.
- Middle Cerebral Artery (MCA) Doppler: Helps in evaluating the redistribution of blood flow (brain-sparing effect) in fetuses with IUGR.
- The Fetal Cardiovascular Profile Score (CVPS) is a comprehensive tool used to evaluate fetal cardiac function and overall well-being in pregnancies at risk for complications.
8. Clinical Management Based on Ductus Venosus Findings:
- Increased Surveillance: Abnormal ductus venosus findings often lead to increased monitoring, including more frequent ultrasounds, biophysical profiles, and non-stress tests.
- The decision for Delivery: Persistent or worsening abnormalities in the ductus venosus waveform may prompt early delivery, especially in the presence of other signs of fetal compromise.
Summary:
The ductus venosus Doppler waveform is a critical part of fetal monitoring, particularly in the second trimester and beyond. Understanding the normal ranges and recognizing abnormal patterns can help clinicians make prompt and informed decisions, improving fetal outcomes.
