Introduction
In recent years, research has provided new insights into fetal heart rate (FHR) values and their variations during gestation. Traditionally, clinicians have relied on standardized thresholds to assess fetal well-being. However, emerging studies highlight how conditions like Long QT Syndrome (LQTS) can disrupt these norms, emphasizing the need for a more nuanced approach to interpreting FHR.
Why Is Long QT Syndrome Important?
- Long QT Syndrome (LQTS) is a genetic cardiac arrhythmia that affects approximately 1 in 2000 individuals.
- LQTS can manifest as complex arrhythmia during fetal life, neonatal, or later in life leading to adverse outcomes. Medication and monitoring can prevent these adverse events.
- During gestation, LQTS can manifest as bradyarrhythmia, characterized by a slower-than-usual heart rate.
The Role of FHR in Detecting LQTS
- A longitudinal study titled “Fetal Heart Rate Predictors of Long QT Syndrome” investigated the use of gestational age-specific percentiles to detect LQTS.
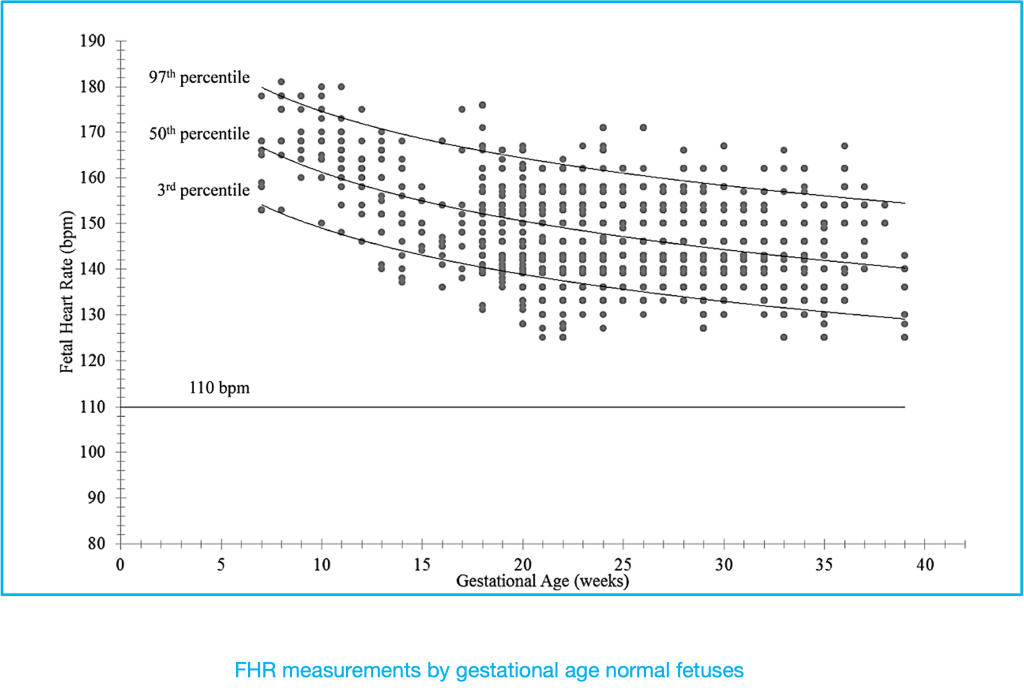
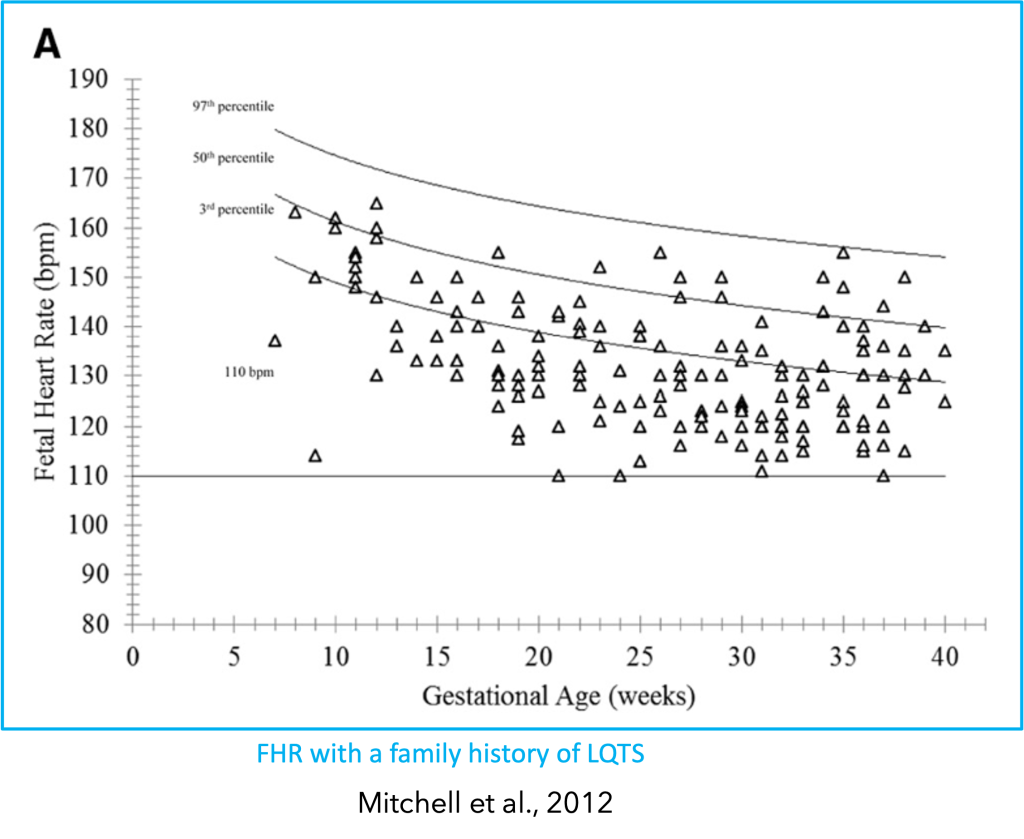
- Findings: Similar to normal fetuses, the FHR of LQTS-affected fetuses decreases with gestational age but consistently remains lower than that of normal fetuses.
- Redefining Bradycardia: By defining bradycardia as an FHR below or equal to the 3rd percentile for gestational age instead of the traditional 110 beats per minute, LQTS identification significantly improves—from 15% to 85% (Mitchell et al., 2012).
https://doi.org/10.1161/CIRCULATIONAHA.112.114132
Additional Marker: Normalized LV Isovolemic Relaxation Time
- Researchers have identified another valuable marker for LQTS detection: the normalized left ventricular (LV) isovolemic relaxation time.
- Thresholds:
- 21-30 weeks: Normalized LV isovolemic relaxation time should be greater than 14.2%.
- >30 weeks: Normalized LV isovolemic relaxation time should be greater than 13.3% (Clur et al., 2018).
- Thresholds:
Genotype-Specific Considerations
- LQT3 Genotype: FHRs of LQT3 genotype-positive fetuses did not significantly differ from those without the familial variant.
- LQT1 and LQT2 Genotypes: Significant variations were observed in the FHRs of fetuses with LQT1 and LQT2 genotypes.
- Severe LQT1 Variants: These variants exhibited lower FHRs compared to mild LQT1 variants (Kaizer et al., 2023).
Why the 3rd Percentile Matters
- Reliable Indicator: An FHR falling below the 3rd percentile for gestational age serves as a more reliable indicator of LQTS than previously established flat rates, and improves LQTS identification—from 15% to 85%. (Mitchell et al., 2012).
- Risk of Complex Arrhythmias: Fetuses with severely lowered FHR are at higher risk of experiencing complex arrhythmias, such as torsades de pointes or 2° atrioventricular block.
- Pre- and Postnatal Concerns: Accurate monitoring is crucial for both pre- and postnatal care.
Conclusion
Understanding FHR dynamics and using gestational age-specific percentiles can enhance LQTS detection. By redefining bradycardia thresholds, clinicians can improve outcomes for both mothers and babies.
—
