Fetal pericardial effusion
- Normal acceptable pericardial fluid thickness is ≤2mm, present in either systole or diastole.
- A fluid collection of 2-4 mm is considered a small pericardial effusion.
- A fluid collection of >4 mm is considered a large effusion.
Normal Pericardial Fluid
The heart is covered by a two-layered membrane all around: the parietal (outer) and visceral (inner) pericardium. The fluid present between the two layers allows a frictionless and smooth motion of the heart during the cardiac cycle. The pericardial fluid moves in the pericardial cavity in sync with the cardiac cycle, moving away from the expanding chambers. This movement of fluid can be documented by echo doppler
The normal pericardial fluid thickness was described by Jeanty et al in 1984 as 2mm, it still holds.
“The normal amount of pericardial fluid in the newborn infant is considered not to exceed 2 to 4 ml. If this amount surrounds a 60 by 40 by 40 mm heart (term fetus), the thickness of the fluid layer would be about 0.8 mm. If this fluid is allowed to accumulate on one side only, then twice the thickness can be expected, for instance, 1.6 mm, which is in the range of what we observed, 1 to 2 mm.” (Jeanty et al).
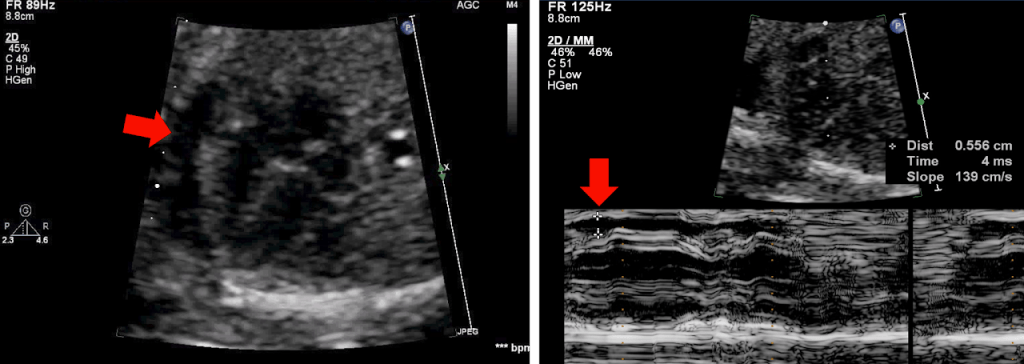
Fetal Echo image showing pericardial effusion(red arrow). 2-D and M-mode images showing the pericardial collection. The maximum diameter is measured irrespective of systole or diastole.
Fetal Pericardial Effusion can be divided into three categories:
- Pericardial Effusion with Hydrops fetalis
- Pericardial Effusion with no Hydrops Fetalis, with anomalies
- Isolated pericardial Effusion
Isolated pericardial effusion
Isolated pericardial effusion is where there is no hydrops so far and essential investigation has not revealed a cause for pericardial effusion. An isolated pericardial effusion has a good prognosis even with a larger amount of effusion.
The chromosomal anomalies were reported in 20-30% of cases of Isolated pericardial effusion, especially Trisomy 21. Thus, the fetus should have a genetic evaluation directed towards an aneuploidy marker especially Down Syndrome. Recent studies showed a lower incidence of trisomy associated with Isolated pericardial effusion, due to universal triple marker screening.
Hydrops Fetalis
The prenatal diagnosis of hydrops fetalis on ultrasound was made with two or more of the following fetal findings:
●Ascites
●Pleural effusion
●Pericardial effusion
●Generalized skin edema (skin thickness >5 mm)
The polyhydramnios is defined as a single deepest pocket of ≥8 cm or an amniotic fluid index of ≥24 cm. A placental thickness of ≥4 cm in the second trimester and of ≥6 cm in the third trimester is considered abnormal.
Causes of Fetal pericardial effusion
The common causes are-
- Heart Failure
• Congenital heart defects
• Valve Regurgitation
• Fetal Tachyarrhythmia.
• Fetal Bradyarrhythmia and Heart Block
• Myocarditis
• Premature Ductus Arteriosus Closure
• Restrictive Foramen Ovale
• Absent Ductus Venosus
• Cardiac Tumours
• Twin-to-twin transfusion
• AF malformations & fistulas and highly vascular tumours - Infections: Viral Myocarditis, CMV, Parvovirus, TORCH, and others.
- Maternal Inflammatory disease
- Fetal anaemia
• Immune and Non-Immune - Malformations and Chromosomal abnormalities
- Lymphatic Dysplasia
- Thoracic malformation – CCAM, Diaphragmatic hernia,
- Tumours
- Urinary Tract Malformation
- Idiopathic
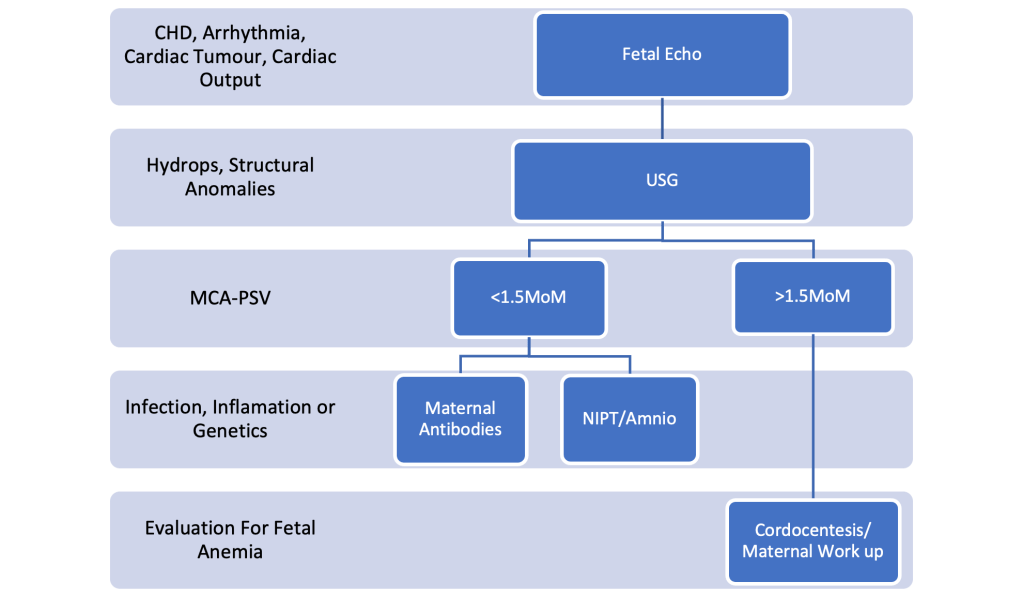
Approach to pericardial collection
Effect of Fetal Pericardial Effusion
Besides the effect of the cause of the pericardial effusion on fetal growth, a progressive large pericardial effusion increases the venous pressure and leads to generalized edema called hydrops. Thus, the pericardial effusion can be part of the hydrops and initiate the hydrops.
A large pericardial effusion occupies significant volumes in the thorax and directly affects the development of the lung and causes pulmonary hypoplasia.
Management
Following up on a patient with fetal pericardial effusion typically involves:
- Regular prenatal ultrasound or echo to monitor the size and amount of fluid in the pericardial sac.
- Evaluating the patient’s overall fetal growth, amniotic fluid volume, and the condition of the placenta.
- Checking for any signs of cardiac distress or changes in the fetal heart rate pattern.
- Performing non-stress tests, biophysical profiles, or other fetal monitoring tests as needed. Umbilical vein pulsation in doppler is useful to monitor and it correlates well with the outcome.
- A team approach between a maternal-fetal medicine specialist or a pediatric cardiologist, an obstetrician and a neonatologist to determine the best course of action, which may include delivering the baby early or preparing for post-birth treatment.
- Closely monitoring the patient after delivery to ensure proper management of the pericardial effusion and any related complications.
Treatment
Management of fetal pericardial effusion involves the treatment of causative mechanisms when identified and treatable.
- Medical management of cardiac arrhythmia.
- Rheumatology reference and management when possible and needed.
- Fetal anemia is treated as per protocol, and intrauterine transfusion whenever indicated.
- Centesis of Pleural effusion, Ascites, Thoracic cystic lesions, or shunt insertion when indicated.
- Open fetal surgery or laser vessel ablation/ radiofrequency ablation for CCAM, Sequestration, Sacrococcygeal teratoma, and Twin-to-twin transfusion syndrome
- Antenatal steroid when premature delivery is expected or planned.
- Cardiac intervention
Cardiac Interventions
- Fetal Pericardiocentesis
The decompression of the pericardial cavity with a large pericardial effusion reduces the risk of fetal hydrops and pulmonary hypoplasia. Pericardiocentesis also helps in prolonging pregnancy till lung maturity. The use of pericardiocentesis before delivery improves ventilation and haemodynamic stability in the preterm infant.
The fetal pericardial effusion due to cardiac tumours such as teratomas and Rhabdomyoma followed closely for the development of hydrops. The target is to be as close to maturity as possible. When the sign of fetal compromise develops before lung maturity, pericardiocentesis can be performed to delay delivery for 1–2 weeks and allow time for the fetus to mature before delivery. Sometimes it might be necessary to repeat the procedure to further the duration of the pregnancy.
Thus the indications for Fetal pericardiocentesis are a large pericardial effusion endangering hydrops, pulmonary hypoplasia or premature delivery in an otherwise uncompromised fetus.
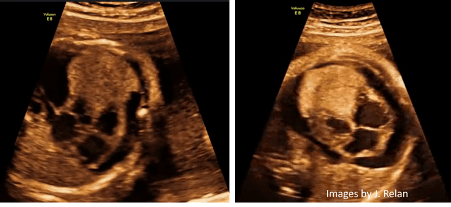
Fetal echo of a 29 weeks fetus showing large Rhabdomyoma causing heart failure and pericardial effusion. A pericardiocentesis was done at the 29th and 33rd weeks and the pregnancy was completed (37 weeks). The baby was given Sirolimus after delivery, and the rhabdomyoma improved. ( JACC: Case Reports Volume 3, Issue 13, 6 October 2021, Pages 1473-1479; Jay Relan et al)
2. Fetal Aortic Valvuloplasty:
Fetal Aortic Valvuloplasty is indicated in a critical AS associated with hydrops. Fetal Aortic Valvuloplasty is also indicated in a critical AS with evolving HLHS and with massive MR, giant left atrium.
3. Fetal Pulmonary Valvuloplasty
Fetal Pulmonary Valvuloplasty is indicated in a critical PS with hydrops and with an evolving right ventricle hypoplasia.
Final word
It’s important to note that the management of fetal pericardial effusion can be complex and may vary based on the severity of the condition and other factors, so close collaboration between obstetricians, fetal medicine specialists and pediatric cardiologists is critical for the best outcomes.
