Persistent left superior vena cava (PLSVC) is the most common systemic venous anomaly. The prevalence of PLSVC ranges from 0.2 to 3% in the general healthy population. Pretorius et al showed in a study of 74 cases that congenital heart defects were present in 4.4% of patients with PLSVC.
In patients with congenital heart disease (CHD), its prevalence ranges between 1.3 and 11%. A prospective study by Ghada S E et al has shown the incidence of PLSVC in CHD is 7.8%. It has the highest association with Coarctation at 27% (5 out of 18 ), followed by AV canal defect and Tetralogy of Fallot, VSD and ASD. In the majority of cases, isolated PLSVC has no clinical implications as venous blood continues to return to the right atrium through the dilated coronary sinus.
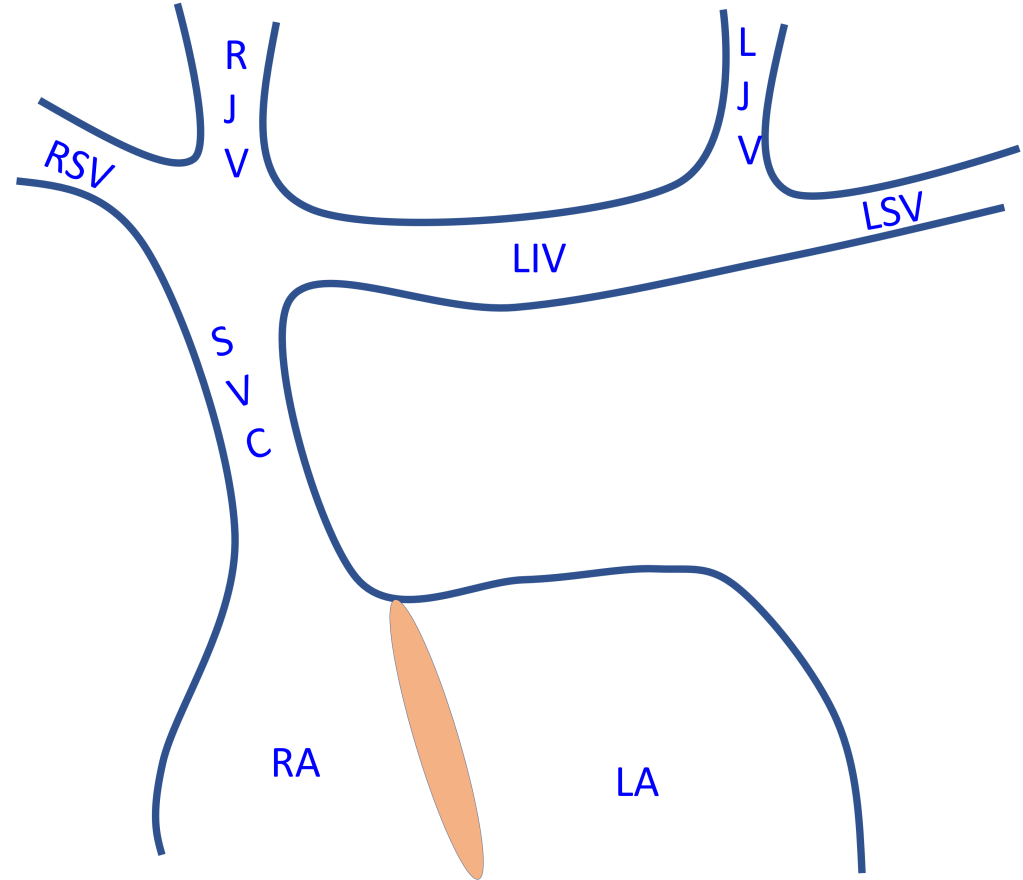
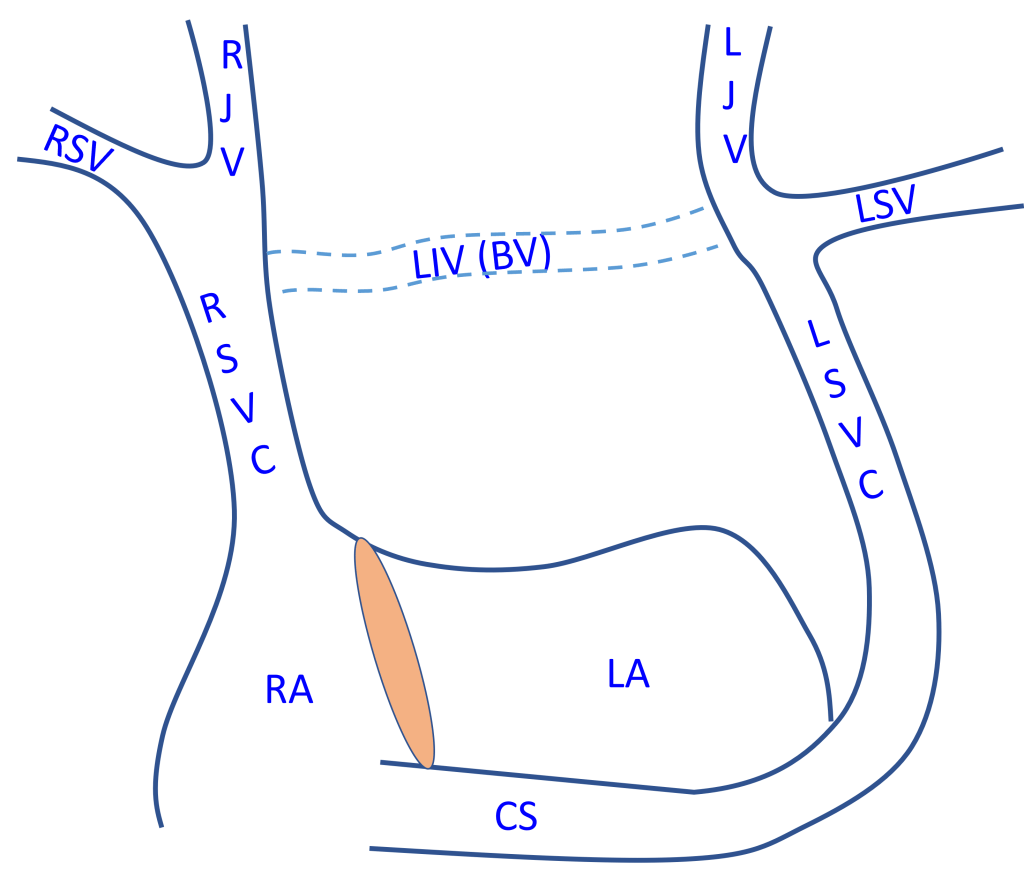
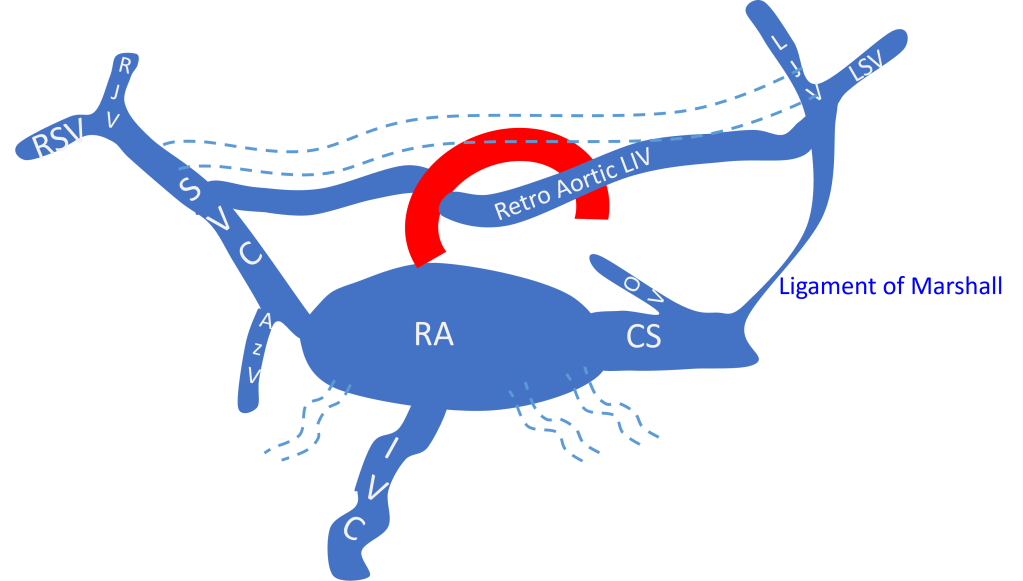
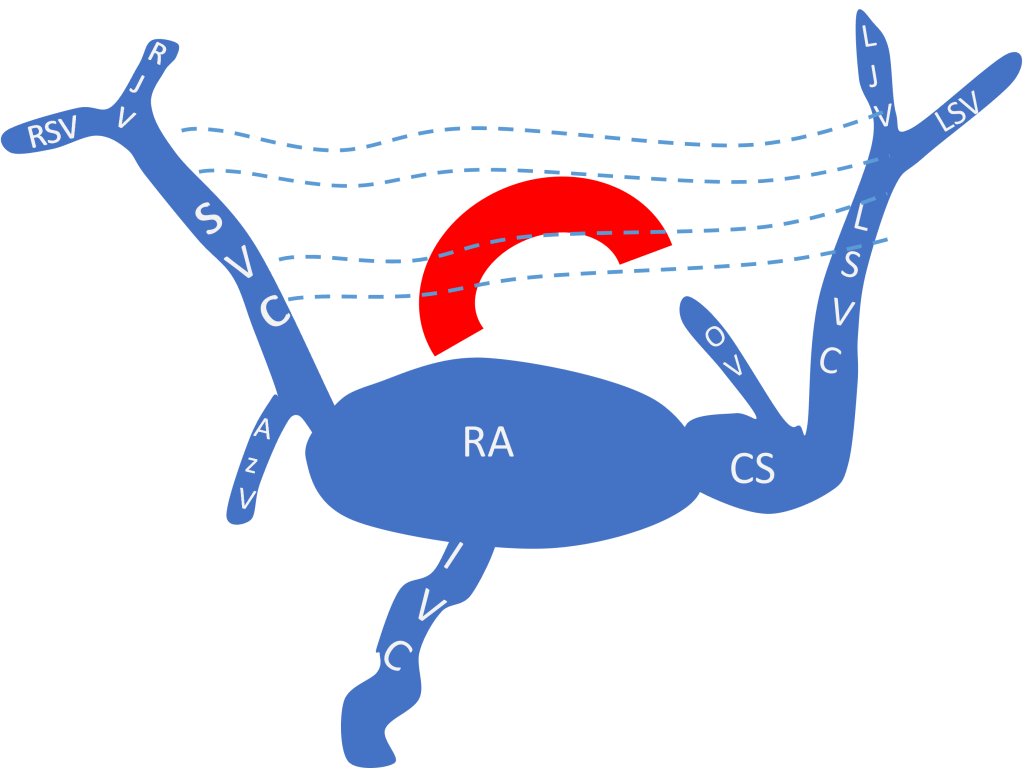
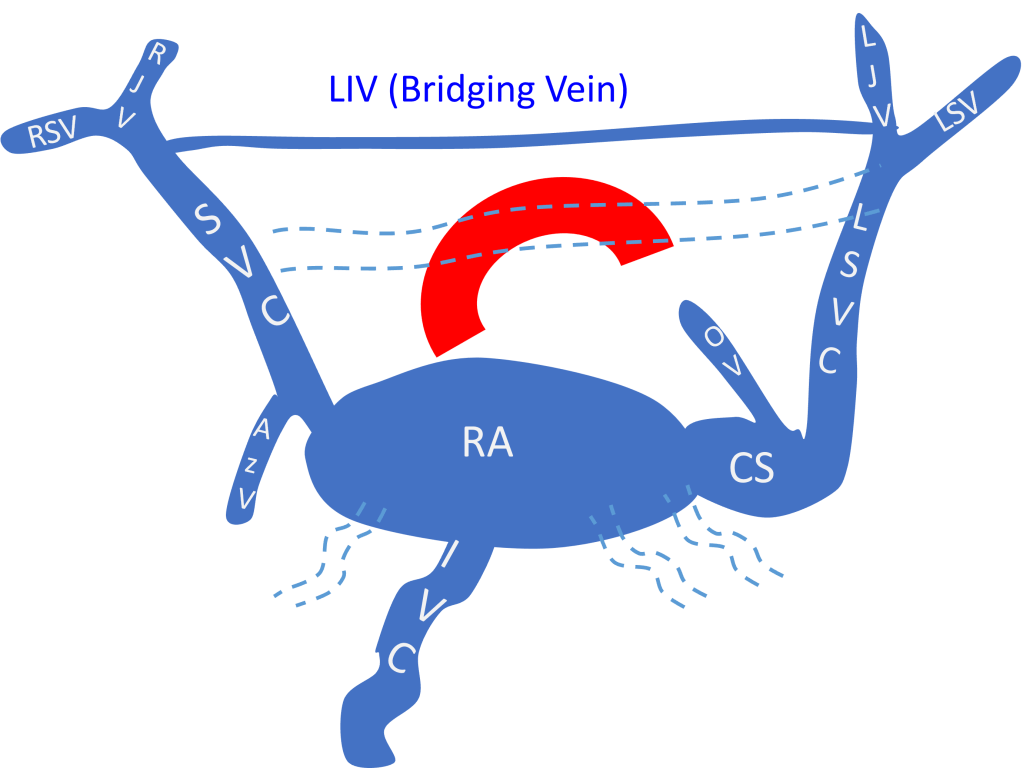
RSV-right subclavian vein, RJV-right jugular vein, LIV-left innominate vein, LJV-left jugular vein, LSV- left subclavian vein, SVC-superior vena cava, RA-right atrium, LA- left atrium, LSVC-left superior vena cava, CS- coronary sinus, BV- bridging vein.
In some cases, PLSVC drains into the LA, due to unroofed coronary sinus causing cyanosis. Rarely with situs solitus also, the PLSVC can be the sole drainage in absence of the right SVC.
Diagnosis of PLSVC
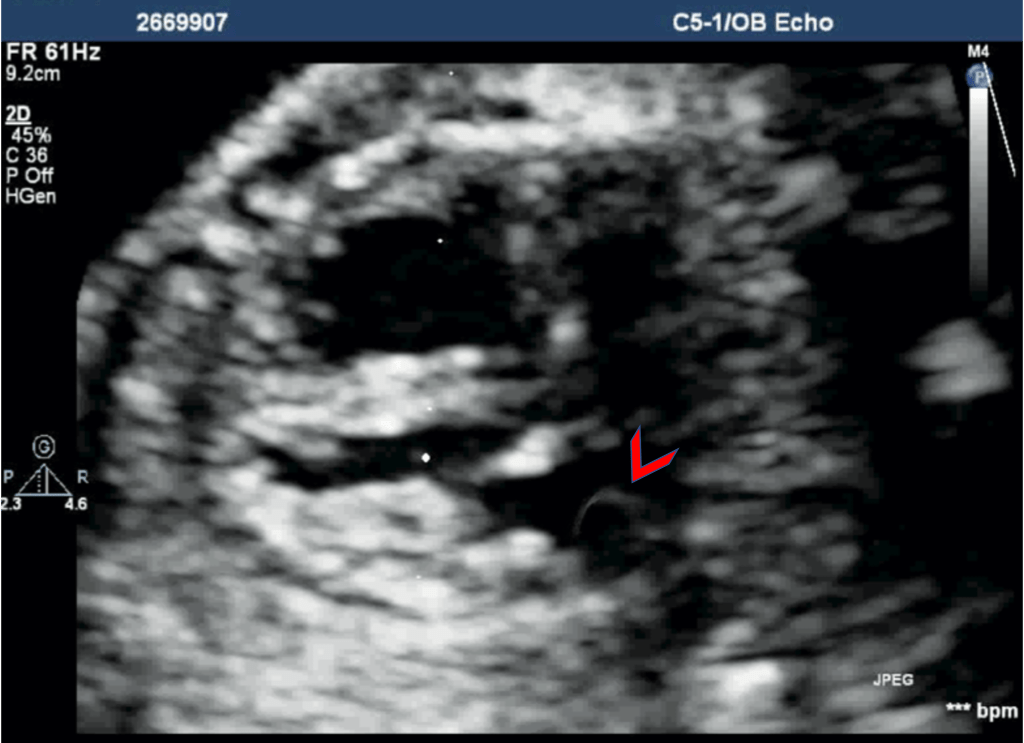
During a neonatal and pediatric echo, screening for PLSVC is part of routine echocardiography. The PLSVC can be direct demonstrated during echo and there is commonly no innominate vein with PLSVC. The drainage of PLSVC to dilated Coronary sinus is present and is well seen from the Apical 4-chamber view.
During the fetal echo, PLSVC is suspected after discovering dilated coronary sinus (CS) and a normal pulmonary venous drainage and then tracing the PLSVC cranially from dilated CS. With the introduction of the three-vessel (3VV) and the three vessels and trachea (3VT) views, PLSVC is diagnosed by the presence of a venous structure left of the pulmonary artery and arterial duct and then tracking caudally to the dilated coronary sinus.

PLSVC Associations
PLSVC can be associated with CHDs and other extra-cardiac anomalies.
A recent meta-analysis by Gustapane et al. of PLSVC in antenatal USG. The occurrence of anomaly has shown that in selected 13 studies with 501 fetuses with PLSVC; 187 fetuses (37.3%) were isolated PLSVC, rest have either intracardiac or extracardiac anomalies.
Chromosomal anomalies occurred in 12.5% with PLSVC overall and with isolated PLSVC, the rate of abnormal karyotype was 7.0%.
Antenatal Coarctation of the aorta was associated with isolated PLSVC in 21.3% and 15.4% have no other sign such as chamber disproportion, however in how many cases the coarctation was confirmed postnatally is not mentioned in the analysis.
The direct inference from this meta-analysis would be that PLSVC is commonly associated with intracardiac or extracardiac anomalies and all fetuses should be well screened after diagnosis of PLSVC. As the incidence of chromosomal anomalies is also found significant thus this can also be considered if there is an additional indication for chromosomal analysis such as significant additional anomalies, family history, past history etc. Like many other studies, it also showed a correlation between the occurrence of PLSVC and Coarctation.
In a meta-analysis by Familiari et al, of Risk Factors for Coarctation of the Aorta on Prenatal Ultrasound, PLSVC did not significantly increase the risk for CoA but PLSVC may represent an independent risk factor for CoA in fetuses not showing any suspicious sign of CoA.
Conclusion:
Persistent Left SVC (PLSVC) is the most common variation of the systemic venous system. Isolated PLSVC has no clinical implications as venous blood return to the right atrium through the dilated coronary sinus. Diagnosis of PLSVC is made when a dilated coronary sinus is seen above the mitral annulus, along with the actual demonstration of LSVC. Studies have shown the coexistence of various cardiac and extra-cardiac anomalies, also an increased incidence of chromosomal anomalies with PLSVC. Association with a coarctation has been shown in meta-analysis and in a few cases, this was the only risk factor.
Embryology of PLSVC
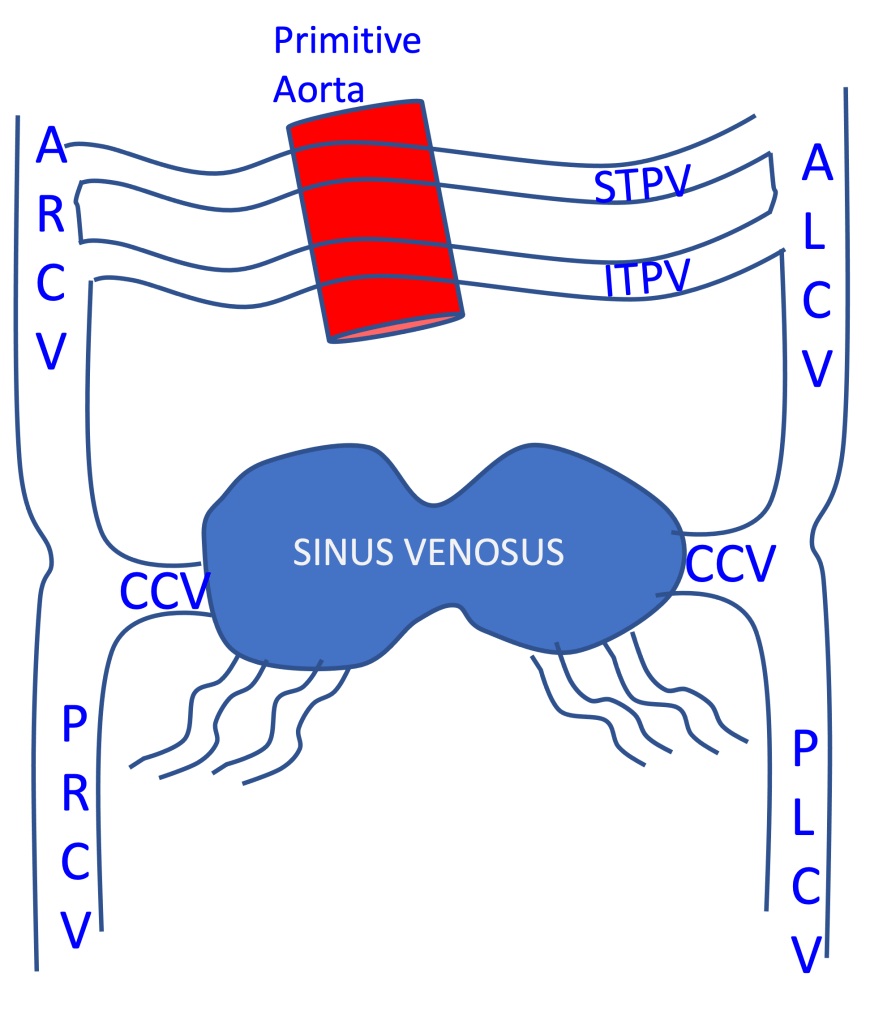
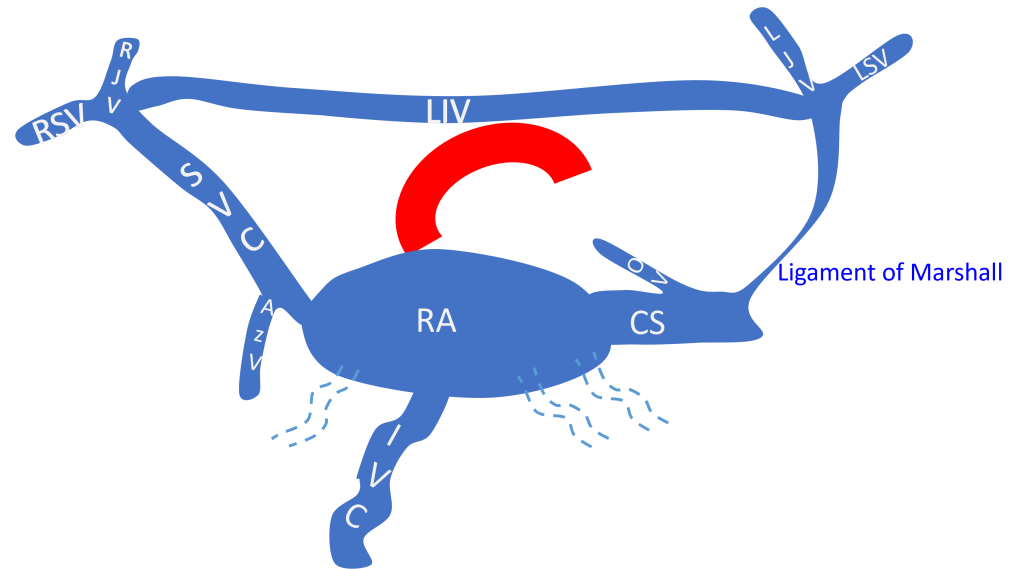
The right VV give rise to the hepato-cardiac segment of the inferior vena cava(IVC), and the left VV with both UV regresses (dashed lines).
The right horn of the sinus venosus merges into the right atrium (RA) evolution, and the left horn becomes the oblique vein of the left atrium (OV) and the coronary sinus (CS).
The STVP grow into the left innominate vein (LIV) while the ITVP regresses (dashed lines) due to the compression by developing the aorta and pulmonary artery.