Ventricle septal defect (VSD) is most common heart defect diagnosed in children and attributed for approximately 30-40 % 0f all congenital heart defects
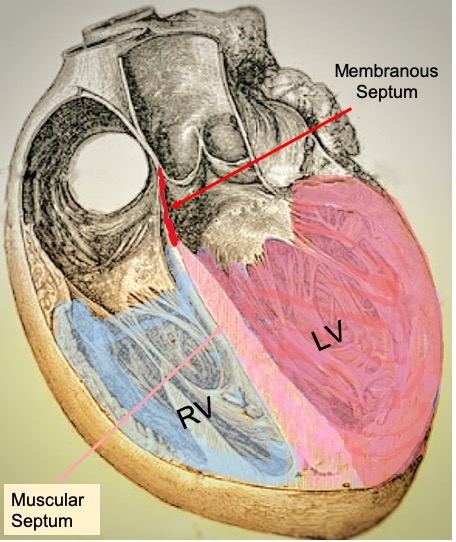
The two ventricles of the heart are separated from each other by a septum, which has the membranous part and the muscular part. The VSD is a septation defect in the septum or a ‘hole’ between the two ventricles of the heart. After birth, the defect in and around membranous septum (perimembranous VSD and sub-arterial VSD) is much more common than the defect in muscular septum (muscular VSD). In contrast, most of the reports have shown in antenatal fetal echocardiography; the muscular septum defects are more frequent (80 vs. 20 %).
These defects are categories as to whether the defect is present in isolation or associated with any other finding in any organ system during ultrasonography. The VSD can also be present in combination with other defects in cardiac structure as well, such as VSD as part of Tetralogy of Fallot, with a right aortic arch or other arch defects, with Valve defects, etc.
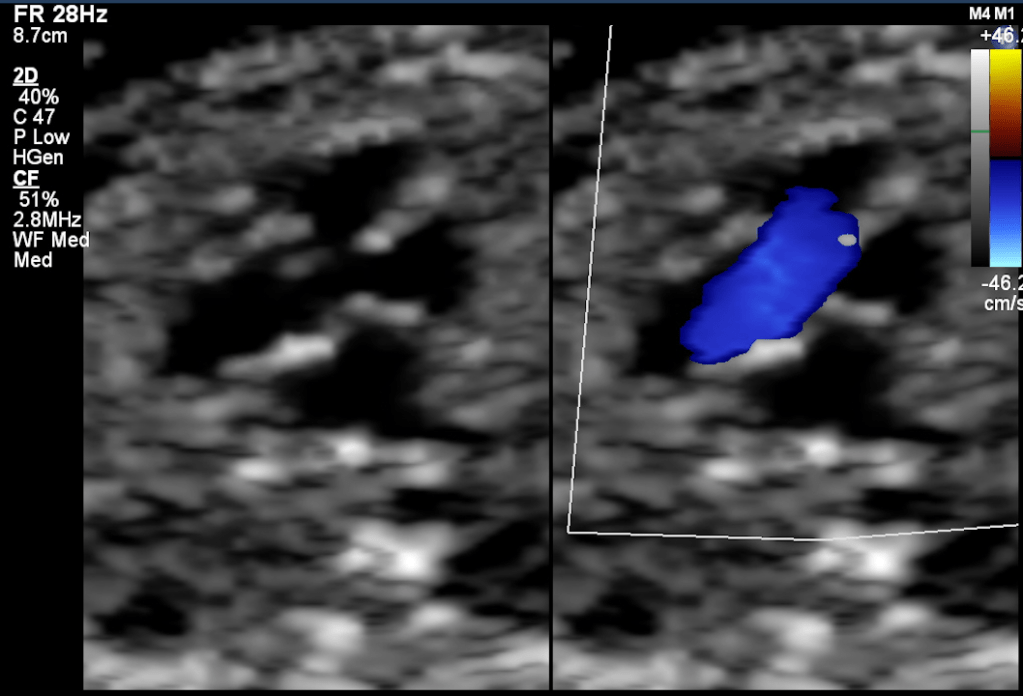
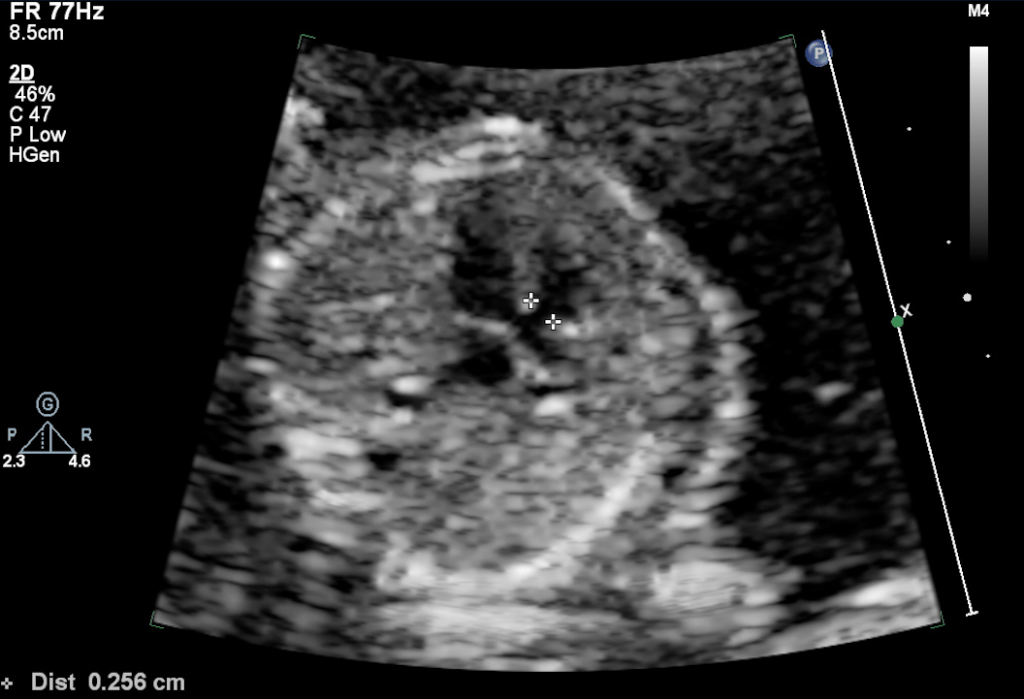
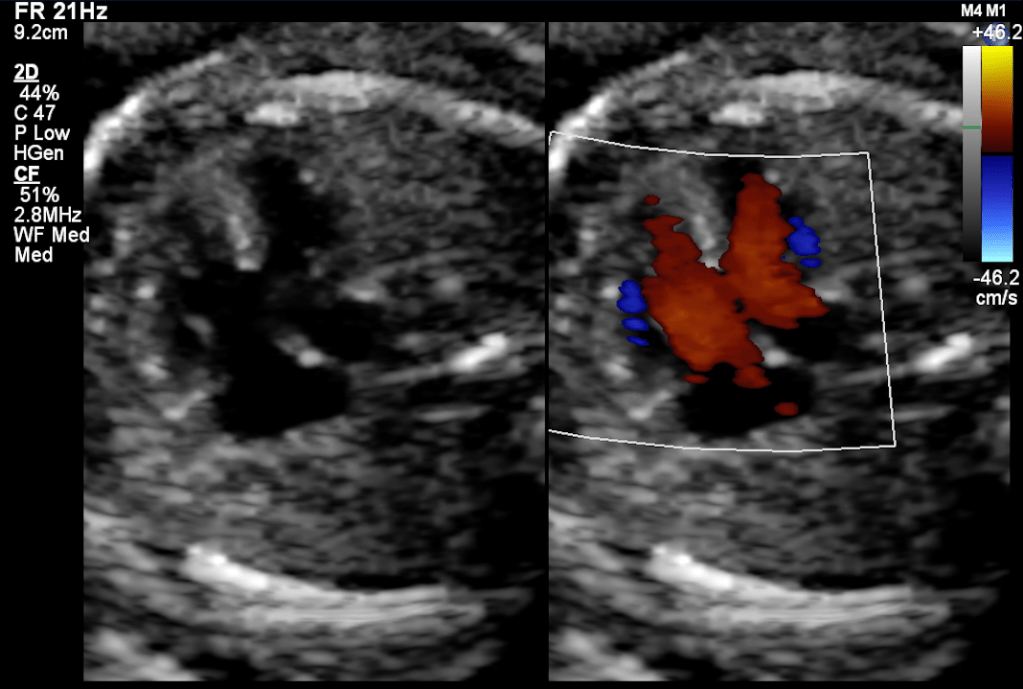
Smaller VSDs are much more common than a large defect. Also, the smaller defects are much more difficult to diagnose in early pregnancy fetal echocardiography because both the ventricle has similar pressures. Thus there is no significant color doppler flow can be seen across small VSD during most of the cardiac cycle. The 2D echo image also can miss a small VSD because of pixel spread of image due to significant magnification used during the echo.
The membranous defects pose a different kind of challenges to diagnoses by fetal echocardiography. This part of the septum is thin thus can appear as drop-out even in the absence of VSD there. Also, during color doppler, the color spill due to increase flow velocity of the outflow tract and great arteries crossover. Thus over-diagnosis is also common, and to avoid over-diagnosis, sometimes the diagnosis can be missed as well.
The presence of additional findings such as Tricuspid regurgitation (TR), Chambers / Arterial size discrepancy, along drop out at the septum might be an indicator of the presence of a ‘true VSD.’
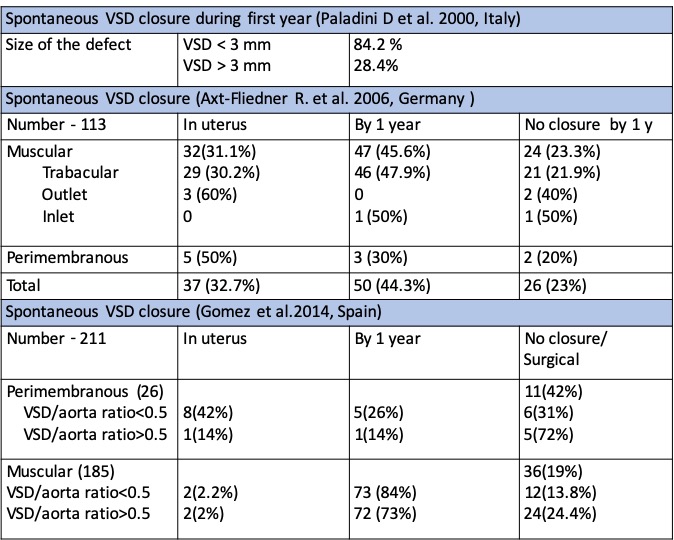
The classification of Large or small VSD is entirely arbitrary, and no classification has been given. From some earlier studies, the outcome has been studied as <3mm and >3 mm size, and closure rate has shown to be different in these two groups. So, it may be fair to use this as classifying the size of the VSD into two groups, viz. small and large VSD. The other criteria used is the ratio of the size of the defect with the annulus size of Aorta. VSD/aorta ratio<0.5 is considered small, and VSD/aorta ratio>0.5 is deemed to be large. Although in many instances there are muscular defects with are seen as definite color drop-out but on 2-D image not measurable, such a defect can be labeled as tiny or very small VSDs or small VSD of < 1mm.
The closure rate of VSD varies depending on the location of VSD, Size of VSD, Time of Diagnosis of the defect, associated cardiac structural defect, and related systemic association. VSDs of larger size, perimembranous and sub arterial location, diagnosed late in gestation, and associated with other cardiac and non-cardiac defects are a lesser chance of closure. When the VSD is part of complex congenital heart disease, it is not expected to close, and it is rather required to maintain hemodynamic antenatally and postnatally.
While all the pediatric series have reported perimembranous defects accounting for approximately 75% of all the VSDs, the muscular VSDs represented the vast majority of cases diagnosed at the antenatal echo. The difference is likely to reflect the high rate of spontaneous resolution of muscular VSDs.
Genetic association with VSD
There is significant concern regarding the association of genetic/chromosomal abnormalities with antenatal detection of VSD, since, with smaller VSDs, there are hardly any hemodynamic consequences before or after birth. Most of the VSDs large or small, either get closed or can be closed after birth if and when required, with < 2% risk with a normal long-term outcome similar to any other child. So the factor which can change the outcome is the presence of other system anomalies and genetic/syndromic association.
Most of the studies have shown no significant or low rate of association with isolated VSD with no extracardiac anomalies. The perimembranous VSD has found to be associated with genetic abnormalities in a few studies. However, still, genetic screening after diagnosis of a perimembranous VSD is not recommended as a routine. Few indications for genetic testing in isolate VSD could be increased maternal age, growth retardation, presence of multiple echogenic foci, presence of aberrant subclavian, small or absent thymus, and presence of aneuploidy in the previous child.When the studies have reported VSD without differentiating isolated from others, then the association rates have been in a range of 25-30 %.
Conclusion
Ventricle Septal Defect (VSD) is the most common cardiac defect diagnosed on antenatal/pediatric echocardiogram. The most common type of defects diagnosed in fetal echocardiogram is the muscular type of defects, most commonly small and ‘isolated.’ Small VSDs have a high closure rate, especially if present at the muscular septum. Isolated small VSDs are rarely associated with genetic anomalies and require genetic screening only in specific indications.
