Isolated complete heart block (CHB) is an immunological disorder in most cases. Mothers of affected fetuses often suffer from connective tissue – autoimmune disease (commonly Sjögren’s syndrome or Systemic lupus erythematosus), but most women may be clinically asymptomatic. However, almost all of them test positive for Anti-nuclear antibodies (ANA) and autoantibodies to the SSA/Ro or SSB/La ribonucleoproteins. These autoantibodies cross the placental barrier and have been shown to react with fetal cardiac tissue, specifically maturing AV node and /or myocardium. Other factors predisposing to the inflammation even in the presence of antibodies in the fetus are not well known as CHB reported in one of the identical twins with similar antibodies in both.
The risk for a woman with known anti-SSA/Ro or anti-SSB/La antibodies to have a child with complete heart block is only about 2 – 5 %. After having had one child with a complete heart block, the recurrence rate is approximately 15 – 20 % in subsequent pregnancies. Autoimmune complete heart block develops between 16 and 24 weeks of gestation in most instances.
The pre and perinatal course and the outcome at the end of the neonatal period largely depend on the presence of fetal hydrops. In several studies, about 75 % of fetuses with isolated complete heart block survived the neonatal period, and almost all of them did not exhibit fetal hydrops. A slow ventricular escape rate (< 55 beats/min) appears to be a poor prognostic factor and a poor ventricular function or endocardial fibroelastosis.
Untreated fetuses with isolated CHB have perinatal mortality of up to 40%. Risk factors for adverse outcomes include fetal hydrops, endocardial fibroelastosis (EFE), a ventricular rate below 55 /min and premature delivery. It is not uncommon to diagnose antibody-mediated myocarditis, hepatitis and dilated cardiomyopathy after birth in the baby with SLE in the mother. This is the basis for treatment in a fetus with CHB and improves the outcome after treatment. However, concerns about toxic steroid effects on the developing fetus and survival are often possible without prenatal intervention; thus, treatment for all is not an option.
Whom to treat is debatable, and the protocol varies at different institutes. The initial studies have shown a possibility of improvement in the first degree of heart block with Dexamethasone (Dexa) treatment. Still, later controlled studies have demonstrated similar recovery outcomes with or without treatment. Comparable with 2nd-degree heart block, studies have shown a variable result in terms of recovery of the level of conduction block. Thus although most centres are in agreement to treat 2nd-degree heart block with Dexa and IVIG, the counselling regarding improvement should be a guarded one. In CHB or 3rd degree of heart block, the conduction is not expected to improve with the treatment. Still, in this group, treatment is required for fetal hydrops, endocardial fibroelastosis (EFE) and low ventricular rate below 55 /min.
The prophylactic treatment of women with positive anti-Ro/ La antibodies with or without the history of the previous fetus with heart block with Hydroxychloroquine (HCQ) has been beneficial in various studies. A recently published study had shown a reduction of the recurrence of CHB below the historical rate by >50%received with 400 mg daily of HCQ before completion of gestational week 10 and maintained through pregnancy.
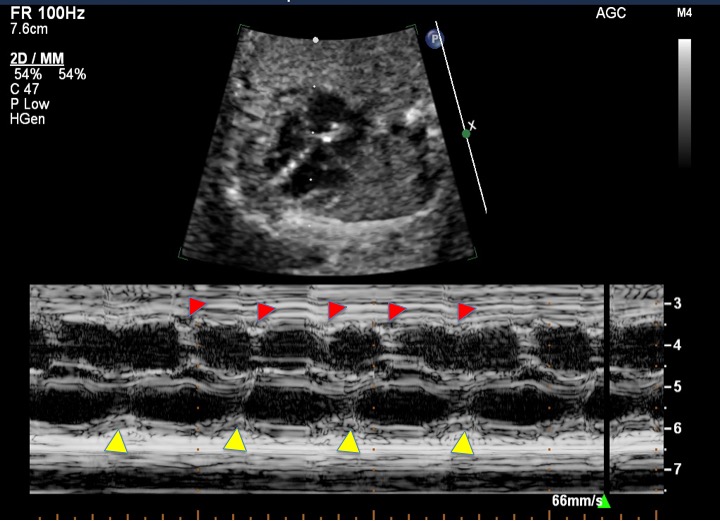
Monitoring of the fetal rhythm in positive anti-Ro/ La antibodies is required. Most centres adopt weekly or biweekly monitoring during high-risk periods and are more liberal during the fringe period. Studies have shown missing early heart block with this protocol. One study has reported a better outcome with home Doppler fetal heart rate monitoring and reporting whenever irregular heart rate is noted on Doppler.
Our Protocol
1. All expectant mothers with positive anti-Ro/ La antibodies with or without a history of the previous fetus with heart block are started on HCQ before pregnancy. If diagnosed later, it is begun on diagnosis at a dose of 200-600 mg (usually 400mg daily). High levels of anti-Ro/SSA or anti- La/SSB (>100U/ml) or high inflammatory markers or clinical signs of disease warrant a higher dose of HCQ or the addition of steroids.
2. All pregnant mothers with positive anti-Ro/ La antibodies with or without the history of the previous fetus with heart block are planned for weekly fetal rhythm monitoring weekly between 16-24 weeks and every other week till 28 weeks. (Home Doppler rate monitoring is not included in our protocol at present)
3. The mechanical PR interval is assessed by the mitral-aorta pulsed-wave Doppler method during the fetal echo. A duration of > 130msec is considered prolonged (+2 z score), and >150 msec (+3 z score) is considered a first-degree heart block. We treat mothers with prolonged PR interval if positive for positive anti-Ro/ La antibodies.
4. If fetal echo shows a 2nd-degree heart block, Dexa and IVIg treatment is also given.
5. If fetal echo shows 3rd-degree heart block, then treatment is given if recent (within 7-10 days), heart rate monitoring has shown heart rate within range and/ or PR interval. Treatment is also offered if fetuses also have fetal hydrops or endocardial fibroelastosis (EFE), even if this is considered established heart block. A low fetal heart rate below 55 /min was also treated with oral salbutamol.
6. Dexamethasone started at 8 mg per day, then reduced to 4 mg per day after two weeks, and then to 2 mg per day at around 30 gestational weeks. Calcium supplementation is given to all mothers, and a ranitidine prescription is given for “as required” administration. The Dexa is tapered after delivery over two weeks for HPA axis suppression. If significant oligohydramnios or uncontrolled diabetes or infection is reported, a reduction or tapering of the Dexa dose is advised.
7. The IVIG is usually administered four times at a dosage of 1 g/kg, within a period of 2 weeks (twice weekly dose). Additional administration is recommended once a month at a dosage of 1 g/kg if the initial treatment time is between the 16th and 30th weeks of gestation.
8. Salbutamol is stated at a dose of 4 mg 6 hourly and increased to 4 hourly if tolerated. In case of significant palpitation, tachycardia, cardiac arrhythmias, hypotension, hyperglycemia, ketoacidosis, and hypokalemia, admission is advised, and the dose is decreased if complications are persistent or life-threatening. An increase of 5 beats /min in fetal heart rate is considered a positive response.
Final word
The Immune Heart Block is partially preventable and possibly treatable if early detection can be done. Detection of a recent change in the level of heart block is desirable, but how frequent check-ups can be done is the limitation. The treatment guidelines are also developing as variable case series showing differences in the outcome with steroid, HCQ, and IVIg treatment. Clinical judgement and discussions between caretaker and patient are very important to plan the line of management.
